Amebiasis Prevention Investment Calculator
Water and Sanitation Impact Calculator
Estimate how your investment in water and sanitation can reduce amebiasis cases and save lives.
Health Outcomes
Economic Impact
Key Insights from the Article
According to the article, in India, a 2019 study calculated an average cost of US$ 45 per case. Bangladesh's 2022 pilot that bundled safe-water filters with school education lowered amebiasis incidence by 38% over two years. The WHO estimates 50 million cases worldwide, with 70,000 deaths annually.
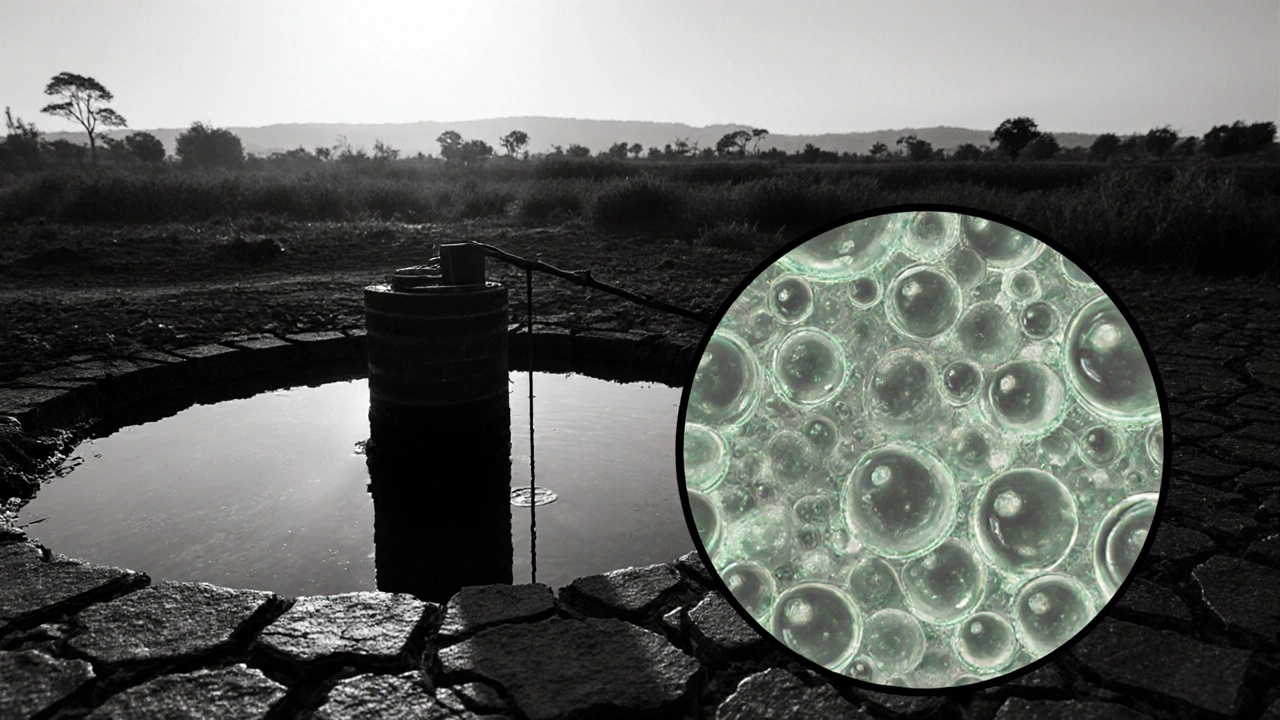
When a parasite slips past a country’s water and sanitation safeguards, it can spark an outbreak that overwhelms clinics and drains budgets. Amebiasis is an intestinal infection caused by the protozoan Entamoeba histolytica. It spreads through contaminated food or water, leading to diarrhea, abdominal pain, and in severe cases, liver abscesses. The disease may seem obscure, but it burdens low‑ and middle‑income nations with millions of cases each year. Understanding how governments intervene can illuminate the broader fight against parasitic diseases.
What is Amebiasis?
Amebiasis primarily affects the colon, where the parasite adheres to the intestinal lining and releases toxins. Symptoms range from mild, self‑limiting diarrhea to dysentery with blood and mucus. About 10% of infected individuals develop extra‑intestinal disease, most often a painful liver abscess. Children and immunocompromised patients are especially vulnerable.
Transmission occurs when people ingest cysts- the hardy, infectious form of Entamoeba histolytica. Cysts survive in untreated water for weeks, cling to raw vegetables washed with polluted water, and can be passed from person to person via poor hand hygiene. The World Health Organization (WHO) estimates roughly 50million cases worldwide, resulting in 70,000 deaths annually.
The Public‑Health Burden
From a Public Health perspective, amebiasis is a classic water‑borne disease that highlights gaps in infrastructure. The disease accounts for an estimated 2.2million disability‑adjusted life years (DALYs) each year, predominantly in South Asia, Sub‑Saharan Africa, and parts of Central America. Outbreaks strain rural clinics, increase antibiotic use, and can trigger school absenteeism, hurting education outcomes.
Beyond health metrics, the economic toll includes direct medical costs (diagnostics, drugs, hospital stays) and indirect losses (lost productivity, caregiving). In India, a 2019 study calculated an average cost of US$45 per case-a sizable amount for households living on less than US$2 a day.
Government Responsibilities: A Multi‑Layered Approach
Effective control hinges on a coordinated government strategy that blends policy, financing, and on‑the‑ground action. Key responsibilities include:
- Surveillance: Establishing national reporting systems to track cases and identify hotspots.
- Water and Sanitation: Investing in safe‑drinking water supplies, sewage treatment, and community latrines.
- Health Education: Running campaigns on hand‑washing, food safety, and proper stool disposal.
- Access to Treatment: Ensuring the supply chain for effective antiparasitic drugs such as Metronidazole and tinidazole.
- Regulation and Quality Control: Monitoring drug quality and preventing counterfeit medicines.
International bodies like the World Health Organization and the Centers for Disease Control and Prevention provide technical guidelines, but national governments must adapt them to local realities.

Prevention Strategies Implemented by Governments
Across the globe, successful programs share common pillars. Below is a snapshot of what many ministries of health have rolled out:
- Provision of chlorine‑based water treatment kits to rural households.
- Construction of community wells protected from surface runoff.
- School‑based hygiene curricula that include hand‑washing after toileting.
- Mass media campaigns using radio jingles in local languages.
- Training of community health workers to identify symptoms early and refer patients.
When these measures are combined, they dramatically cut transmission. In Bangladesh, a 2022 pilot that bundled safe‑water filters with school education lowered amebiasis incidence by 38% over two years.
Treatment Protocols and Government’s Role in Access
The standard regimen for uncomplicated amebiasis is a short course (5‑10days) of amebiasis prevention drug therapy with Metronidazole (or tinidazole) followed by a luminal agent such as paromomycin to eradicate cysts. For invasive disease, higher‑dose intravenous metronidazole plus drainage of liver abscesses is required.
Governments influence treatment outcomes by:
- Negotiating bulk procurement contracts to lower drug prices.
- Integrating amebiasis drugs into essential medicines lists.
- Ensuring that primary‑care facilities have proper diagnostic kits-microscopy, antigen detection, or PCR where feasible.
- Training clinicians on updated WHO treatment guidelines.
In Brazil, a 2021 policy mandated that all public health units stock metronidazole, reducing stock‑outs by 92% and cutting average treatment delay from 7 to 2days.
Case Studies: Lessons from the Field
India’s National Water Mission (2020‑2025) allocated US$1.2billion to upgrade rural water infrastructure. Coupled with an amebiasis awareness drive, case numbers dropped from an estimated 2.4million in 2019 to 1.6million in 2024.
Kenya’s Community Health Volunteer Program trains local volunteers to distribute chlorine tablets and educate families on safe food handling. A 2023 evaluation reported a 27% reduction in diarrheal diseases, including amebiasis, in participating districts.
These examples underscore that political commitment, adequate financing, and culturally tailored messaging create measurable health gains.

Remaining Challenges and Policy Recommendations
Despite progress, several hurdles persist:
- Funding gaps: Many low‑income governments rely on external donors, making programs vulnerable to budget cuts.
- Urban slums: Rapid urbanization outpaces sanitation upgrades, keeping transmission pockets alive.
- Drug resistance: Emerging metronidazole‑resistant strains threaten standard therapy.
- Data limitations: Under‑reporting hampers accurate burden estimation.
Policymakers should consider the following actions:
- Establish a dedicated amebiasis fund within national health budgets.
- Scale up point‑of‑use water filtration technologies in densely populated peri‑urban zones.
- Invest in rapid diagnostic tools to improve case detection and reporting.
- Promote research on alternative drug regimens and potential vaccines.
- Foster cross‑sector collaboration between health, water, education, and finance ministries.
By embedding these steps into national health plans, governments can move from reactionary treatment to sustainable disease control.
Quick Checklist for Government Officials
- ✔️ Have you integrated amebiasis surveillance into existing disease reporting systems?
- ✔️ Are safe‑drinking water sources available to >90% of the at‑risk population?
- ✔️ Do primary‑care clinics stock WHO‑recommended antiparasitic drugs?
- ✔️ Is there a community‑based hygiene education program in schools?
- ✔️ Have you allocated budget for regular drug quality audits?
Checking these boxes can dramatically reduce both incidence and mortality.
Frequently Asked Questions
How is amebiasis diagnosed?
Diagnosis usually starts with stool microscopy to spot cysts or trophozoites. More accurate options include antigen detection kits or PCR assays, which many national labs are beginning to adopt.
Can amebiasis be prevented without advanced infrastructure?
Yes. Low‑cost measures such as household chlorination, boiling water, proper hand‑washing, and cooking vegetables thoroughly can cut transmission dramatically, even in resource‑limited settings.
What is the first‑line drug for amebiasis?
Metronidazole (or tinidazole) taken for 5‑10days, followed by a luminal agent like paromomycin, is the WHO‑recommended first‑line therapy for uncomplicated infection.
Why do some countries report fewer cases than expected?
Under‑reporting stems from limited diagnostic capacity, social stigma, and fragmented surveillance. Strengthening laboratory networks and community awareness often reveals a higher true burden.
Is there a vaccine for amebiasis?
Research is ongoing, but no licensed vaccine exists yet. Governments can support clinical trials and fund basic science to accelerate development.

John Babko
October 16, 2025 AT 12:36Our nation’s water safety should never be compromised – when politicians cut corners on sanitation, the most vulnerable pay the price!! The government must enforce strict standards for drinking water, fund rural well projects, and punish any corruption that jeopardizes public health!!
Stacy McAlpine
October 16, 2025 AT 16:30It’s amazing how a simple hand‑wash routine can save families from a nasty gut infection. Getting the word out in schools, community centers, and on social media can make a massive dent in cases.
Hanna Sundqvist
October 16, 2025 AT 18:26People wnat to think the gov is looking out for us but the real power lies with those who control the water filtrations…they dont tell us about the hidden chemicals they slip into the supply, and thats why the parasite keeps comin back.
Jim Butler
October 16, 2025 AT 20:40Dear colleagues, let us commend the ministries that have integrated amebiasis drugs into essential medicine lists. This decisive action accelerates treatment, reduces mortality, and sets a benchmark for other nations. 😊
Ian McKay
October 17, 2025 AT 00:50The article correctly outlines surveillance, yet it omits the necessity of standardized case definitions across regions. Without uniform criteria, data comparability suffers.
Deborah Messick
October 17, 2025 AT 03:03While many applaud the progress, one must ask whether the allocated funds truly reach the intended projects or are merely reshuffled to satisfy donor requirements. Transparency is the only safeguard against mismanagement.
Renee van Baar
October 17, 2025 AT 05:00When we look at the broader picture of amebiasis control, several interlinked pillars emerge, each demanding attention from policymakers, health workers, and community members alike.
First, reliable surveillance data are the backbone of any effective response; without accurate numbers, resources cannot be allocated efficiently.
Second, water and sanitation infrastructure must be both resilient and adaptable to climate‑induced stresses, ensuring that even remote villages have access to safe drinking water year‑round.
Third, health education cannot remain a one‑off campaign; it needs to be integrated into school curricula, workplace trainings, and local radio programming, using local languages and culturally relevant messages.
Fourth, the supply chain for antiprotozoal medications must be transparent, with regular audits to prevent counterfeit or expired products from reaching clinics.
Fifth, community health workers should receive ongoing mentorship, empowering them to recognize early symptoms and refer patients promptly.
Sixth, we must invest in rapid diagnostic tools that are affordable and easy to use in low‑resource settings, shifting the diagnostic burden away from centralized labs.
Seventh, governments should establish dedicated amebiasis funds within national health budgets, protecting programs from the volatility of donor cycles.
Eighth, urban slums need targeted interventions, such as point‑of‑use filtration devices, because traditional water infrastructure often lags behind rapid population growth.
Ninth, research into alternative drug regimens and potential vaccines should be a priority, especially given emerging resistance patterns.
Tenth, cross‑sector collaboration among health, water, education, and finance ministries ensures that policies are coherent and mutually reinforcing.
Eleventh, continuous monitoring and evaluation of interventions allow for evidence‑based adjustments, maximizing impact.
Finally, public‑private partnerships can mobilize additional resources and technical expertise, accelerating the rollout of innovative solutions.
By embracing this comprehensive, multi‑layered strategy, nations can move from reactive treatment toward sustainable disease control, ultimately safeguarding the health and productivity of their citizens.
Janice Rodrigiez
October 17, 2025 AT 13:20Think of chlorine tablets as the cheap superhero of water safety – they’re cheap, easy to distribute, and knock out parasites fast.
Jonathan Seanston
October 17, 2025 AT 15:33Totally agree! Nothing beats a friendly neighbor showing you how to set up a simple filter at home.
Sukanya Borborah
October 17, 2025 AT 18:53From a policy‑analysis standpoint, the cost‑effectiveness matrix for amebiasis interventions often gets glossed over. The real ROI hinges on scaling low‑tech solutions like household chlorination, which trims not only disease burden but also indirect productivity losses.
Stu Davies
October 17, 2025 AT 21:23It’s heart‑warming to see community volunteers taking charge. Their dedication bridges the gap between clinics and households. 😊
Nadia Stallaert
October 18, 2025 AT 00:26Behold! The hidden agenda of the global health elite-peddling surveillance data while the true pathogen thrives in the shadows of bureaucracy!!! The very frameworks meant to protect us become cages for complacency!!!
Greg RipKid
October 18, 2025 AT 06:00Facts speak louder than hype.
John Price Hannah
October 18, 2025 AT 07:23Oh, the drama of a single‑sentence nugget-so bland, so... *meh*-yet it slices through the noise like a dull butter knife, barely making a dent in the grand narrative of public health negligence!!!