Most people think of painkillers like ibuprofen or acetaminophen as harmless-something you grab off the shelf when your head hurts or your back flares up. But what if taking a few pills every day for years quietly damaged your kidneys? That’s not a hypothetical. It’s analgesic nephropathy, a preventable kidney disease caused by long-term, high-dose use of common pain medications. And it’s happening more than you think.
What Exactly Is Analgesic Nephropathy?
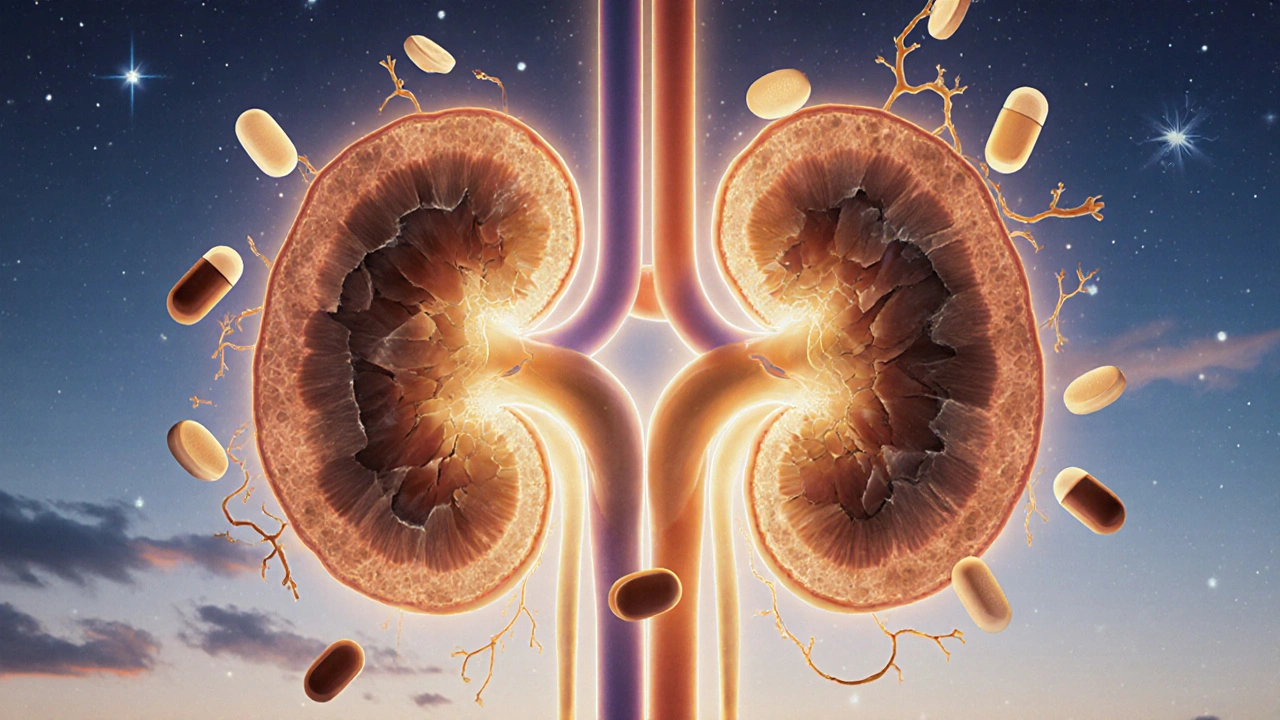
Analgesic nephropathy is a slow, silent injury to the kidneys caused by years of heavy use of painkillers, especially NSAIDs like ibuprofen, naproxen, and aspirin, and sometimes acetaminophen. It doesn’t hit you overnight. It creeps in. You take a few pills daily for headaches, menstrual cramps, or arthritis pain. Over time, those pills start damaging the tiny filtering units inside your kidneys-the nephrons-and the inner lining of the renal pelvis.
The damage shows up as chronic tubulointerstitial nephritis, where the spaces between kidney tubules become scarred. Eventually, this leads to renal papillary necrosis-tissue death in the inner part of the kidney. By the time symptoms appear, the damage is often advanced. And here’s the kicker: many people don’t know they have it until their doctor runs blood tests and finds their kidney function has dropped.
Who’s at Risk?
This isn’t just a problem for older adults. While it’s most common in people over 45, women between 30 and 55 are disproportionately affected. Why? Because they’re more likely to use combination painkillers daily-for migraines, endometriosis, fibromyalgia, or chronic back pain. A 2021 study found that 72% of diagnosed cases were women.
The biggest risk factor? Taking 6 or more pills a day for 3 or more years. That might sound extreme, but it’s not rare. Think about someone who takes 2 Excedrin Migraine tablets (each with 65 mg caffeine, 250 mg acetaminophen, and 250 mg aspirin) three times a day. That’s 18 pills a week. Over five years, that’s more than 4,500 pills. That’s the kind of usage that leads to kidney damage.
And it’s not just the amount-it’s the mix. Combination products with caffeine or codeine are 3.7 times more likely to cause kidney injury than single-ingredient painkillers. Even though phenacetin (a once-common ingredient in combo pills) was banned in the 1980s, the same pattern continues today with caffeine-laced OTC pain relievers.
How Do NSAIDs Actually Hurt Your Kidneys?
NSAIDs work by blocking enzymes called COX-1 and COX-2, which reduce inflammation and pain. But those same enzymes help keep blood flowing to your kidneys. When you take NSAIDs regularly, your kidneys get less blood. That’s not a side effect-it’s the direct result.
At normal doses, NSAIDs can reduce kidney blood flow by 25-40%. At higher doses, that drops to 50-70%. Your kidneys respond by holding onto sodium and water, which raises blood pressure. Over time, this leads to scarring, loss of filtering ability, and eventually, chronic kidney disease.
Acetaminophen is often seen as the “safe” alternative. But a 2020 study in Kidney International Reports found that people who took more than 4,000 mg of acetaminophen daily for five or more years had a 68% higher risk of developing chronic kidney disease than non-users. It’s not harmless-it’s just slower to damage.

How Is It Diagnosed?
Most people don’t feel anything until their kidneys are already damaged. Early signs are invisible: fatigue, mild swelling in the ankles, or slightly elevated blood pressure. The first real clue? A routine blood test showing a rising creatinine level or a drop in GFR (glomerular filtration rate).
Doctors look for:
- Non-nephrotic proteinuria (less than 3.5 grams of protein in urine per day)
- Bland urinary sediment (no red blood cells or casts)
- Sterile pyuria (white blood cells in urine without infection)
Imaging helps confirm it. A noncontrast CT scan can show calcifications in the renal papillae-with 87% sensitivity and 97% specificity. But here’s the good news: a new FDA-approved urine test called NephroCheck, launched in January 2023, can detect early signs of papillary damage with 92% accuracy. That means you might catch it before it’s too late.
What Happens If You Don’t Stop?
Left unchecked, analgesic nephropathy leads to irreversible kidney failure. You’ll develop high blood pressure, anemia, and trouble concentrating urine. Eventually, you may pass pieces of dead kidney tissue (papillae), which can block your urinary tract and cause severe pain.
At the end stage, you’ll need dialysis or a kidney transplant. In the U.S., analgesic nephropathy contributes to 15,000-20,000 new chronic kidney disease cases each year. The annual cost? Up to $90,000 per patient on dialysis. That’s preventable suffering-and preventable expense.
What’s the Real Problem? Misconceptions
A 2022 Cedars-Sinai survey found that 62% of patients diagnosed with analgesic nephropathy didn’t believe OTC painkillers could harm their kidneys. They thought, “It’s just a pill.” But here’s the truth: the FDA mandated stronger kidney risk warnings on all NSAID labels in 2020. The warnings are there. Most people just don’t read them.
And doctors aren’t always proactive. The National Kidney Foundation recommends checking creatinine levels every 6 months for anyone on chronic pain meds. But in real-world practice, that rarely happens unless the patient brings it up.
Safer Pain Control: What Actually Works
The good news? You don’t have to suffer. There are effective, kidney-safe ways to manage chronic pain.
1. Start with Non-Drug Options
The American College of Rheumatology recommends trying physical therapy, heat therapy, or cognitive behavioral therapy for 4-6 weeks before turning to pills. Heat wraps like ThermaCare have been shown to reduce osteoarthritis pain by 40-60% without any kidney risk. Acupuncture and tai chi also show strong evidence for chronic pain relief.
2. Use Topical NSAIDs
If you need an NSAID, skip the pills. Use a gel or patch. Topical diclofenac reduces systemic exposure by 90%. A 2021 study in Arthritis & Rheumatology found it worked just as well as oral ibuprofen for joint pain-with zero decline in kidney function after 12 weeks.
3. Stick to Strict Limits
If you must take oral NSAIDs:
- Never exceed 1,200 mg of ibuprofen per day
- Never exceed 750 mg of naproxen per day
- Use them for no more than 10 consecutive days without seeing a doctor
- Avoid daily use unless absolutely necessary
For acetaminophen, cap it at 3,000 mg per day-never 4,000 mg. That’s the new FDA-recommended limit for long-term safety.
4. Try Alternatives
For migraines: CGRP inhibitors like Aimovig or Emgality are prescription-only, cost around $650/month, but carry zero kidney risk. For mild pain: CBD products at doses under 1,500 mg/day show no kidney toxicity in a 2022 JAMA study. Not a miracle cure, but safer than daily NSAIDs.
What to Do If You’ve Been Taking Painkillers Daily
If you’ve been using NSAIDs or acetaminophen every day for 3+ years:
- Get a blood test for creatinine and calculate your eGFR.
- Ask for a urine test to check for protein or white blood cells.
- If you’re over 45, have high blood pressure, or have diabetes, get tested even if you feel fine.
- If your kidney function is low, stop NSAIDs immediately and work with your doctor on alternatives.
Here’s the hopeful part: a 2022 study in the Clinical Journal of the American Society of Nephrology followed 142 people who stopped their painkillers after early diagnosis. Seventy-three percent stabilized their kidney function. No further decline. No dialysis. Just stopping the meds and switching to safer strategies.
Bottom Line
Analgesic nephropathy isn’t a rare disease. It’s a consequence of how we treat pain in modern life. We treat symptoms without asking what’s causing them. We reach for pills because they’re easy. But our kidneys pay the price.
You don’t need to live with pain. But you do need to be smarter about how you manage it. Stop assuming OTC painkillers are safe for long-term use. Start asking your doctor about alternatives. Get your kidneys checked if you’ve been on daily pain meds. And remember: the best pain relief isn’t always a pill-it’s the right strategy, used early, before damage sets in.

Matthew McCraney
November 19, 2025 AT 17:23soooooo the gov is hiding this?? ibuprofen is a bioweapon disguised as a headache pill?? i knew it!! my cousin's neighbor's dog got kidney failure after licking a spilled Advil bottle and now the whole block is on cia surveillance. they dont want us to know that the pharmaceutical giants are secretly running kidney farms in the desert. also, acetaminophen is just powdered moon rocks from the alien base in Area 51. check the label next time you buy it-see the tiny 'NSAID-17' code? thats the tracking chip. i stopped taking pills and now i just scream into a pillow. my kidneys are thanking me. 🤫💊
serge jane
November 21, 2025 AT 00:23its fascinating how we treat pain like a bug to be eradicated rather than a signal to be understood. we live in a culture that equates comfort with health and silence with victory. the body speaks in pain and we answer with chemicals. we dont ask why the back hurts we just mute the alarm. the kidneys dont care about your schedule or your deadlines they just filter what you pour into them. every pill is a vote for how you treat your own biology. maybe the real problem isnt the medication its the assumption that pain is an enemy instead of a messenger. we need to listen before we suppress. and maybe then we wont need so many pills in the first place
Rusty Thomas
November 21, 2025 AT 02:30OMG I JUST REALIZED I’VE BEEN TAKING EXCEDRIN SINCE 2018 😭 I thought I was being responsible because I only took 2 a day… TWO A DAY?? FOR SIX YEARS?? MY KIDNEYS ARE PROBABLY WRITING ME A LETTER IN BLOOD RIGHT NOW. I’m crying. I’m calling my doctor. I’m throwing out my medicine cabinet. I’m switching to yoga and crying into my chamomile tea. 😭🫂 #painkillersarenotfriends
Sarah Swiatek
November 21, 2025 AT 12:47lets be real-nobody reads the fine print until their kidneys start screaming. i used to think acetaminophen was the ‘safe’ option because my grandma said so. turns out grandma was right about a lot of things but not about dosage limits. the fact that the FDA updated warnings in 2020 and still 62% of patients didn’t know? that’s not ignorance. that’s systemic neglect. doctors dont have time. pharmacies dont remind you. the system is designed to keep you medicated and quiet. the real miracle isn’t the new urine test-it’s that anyone survived this long without knowing. topicals? yes. physical therapy? yes. stopping? absolutely. but the real win? realizing you dont need to suffer to be strong. sometimes strength is knowing when to put the pill down
Lemmy Coco
November 22, 2025 AT 04:33i had no idea about the 6 pills a day thing… i thought i was fine cause i only took 1 or 2 when i needed it. but then i realized i was taking them almost every day for 4 years… oops. i just checked my creatinine last week and it was a little high. im gonna try the topical diclofenac. also i think i might have a problem with self-medicating. sorry for the typos. my hands are shaking a little
rob lafata
November 22, 2025 AT 12:16you people are such sheep. you swallow whatever the pharma bros feed you like it’s gospel. NSAIDs? they’re just the gateway drug to dialysis. and dont even get me started on acetaminophen-thats liquid betrayal wrapped in a blue capsule. the FDA? they’re owned by Big Pharma. the ‘new’ urine test? a marketing ploy to sell more tests. the real solution? stop trusting anyone who wears a lab coat and charges you $150 for a 5-minute consult. go herbal. go fasting. go primal. go off-grid. your kidneys will thank you. and if they dont? well. you were warned. #pharmaindustrylies
Nick Naylor
November 23, 2025 AT 04:56Brianna Groleau
November 25, 2025 AT 03:01i grew up in a household where pain meant ‘suck it up’ or ‘take two aspirin’-no questions asked. i never thought about how my body was holding up. now that i’m 38 and my ankles swell after walking to the mailbox, i realize i’ve been punishing my kidneys for a decade. i started using heat wraps for my lower back and honestly? they work better than ibuprofen ever did. i feel warmer. i feel calmer. i feel like i’m not poisoning myself. i used to think natural was weak. now i know it’s wise. and if you’re reading this and you’ve been popping pills like candy… you’re not weak. you’re just tired. and it’s okay to ask for help. you deserve to feel better without breaking your body
Dave Wooldridge
November 26, 2025 AT 19:36they’re putting fluoride in the water and NSAIDs in the painkillers so we all get kidney failure by 50. then they sell us dialysis machines. it’s all planned. the same people who make the pills make the transplants. they want you dependent. they want you in debt. they want you too weak to protest. the ‘new’ urine test? it’s just a trap to get you to pay for more tests. they don’t want you to heal. they want you to pay. i stopped all meds. now i drink lemon water and stare at the moon. my kidneys are healing. i can feel it. they’re whispering to me. they’re grateful.
Rebecca Cosenza
November 26, 2025 AT 20:503,000 mg max. not 4,000. stop.
swatantra kumar
November 27, 2025 AT 12:27bro i used to take 2 ibuprofen every night for my sciatica… now i do 20 mins of yoga before bed and my pain is way better. also i started drinking turmeric tea with black pepper-tastes like earth and magic. my kidneys feel lighter 😊 no more pills. no more fear. just breath. and a little spice. namaste 🙏