Antidepressant Monitoring Frequency Calculator
How Often Should Your Teen Be Monitored?
Use this tool to determine the recommended monitoring frequency based on treatment duration and risk factors. Follows FDA guidelines for teens on antidepressants.
Recommended Monitoring Plan
- Assess mood and suicidal thoughts at each visit
- Watch for increased agitation or sleep disturbances
- Document any side effects or behavior changes
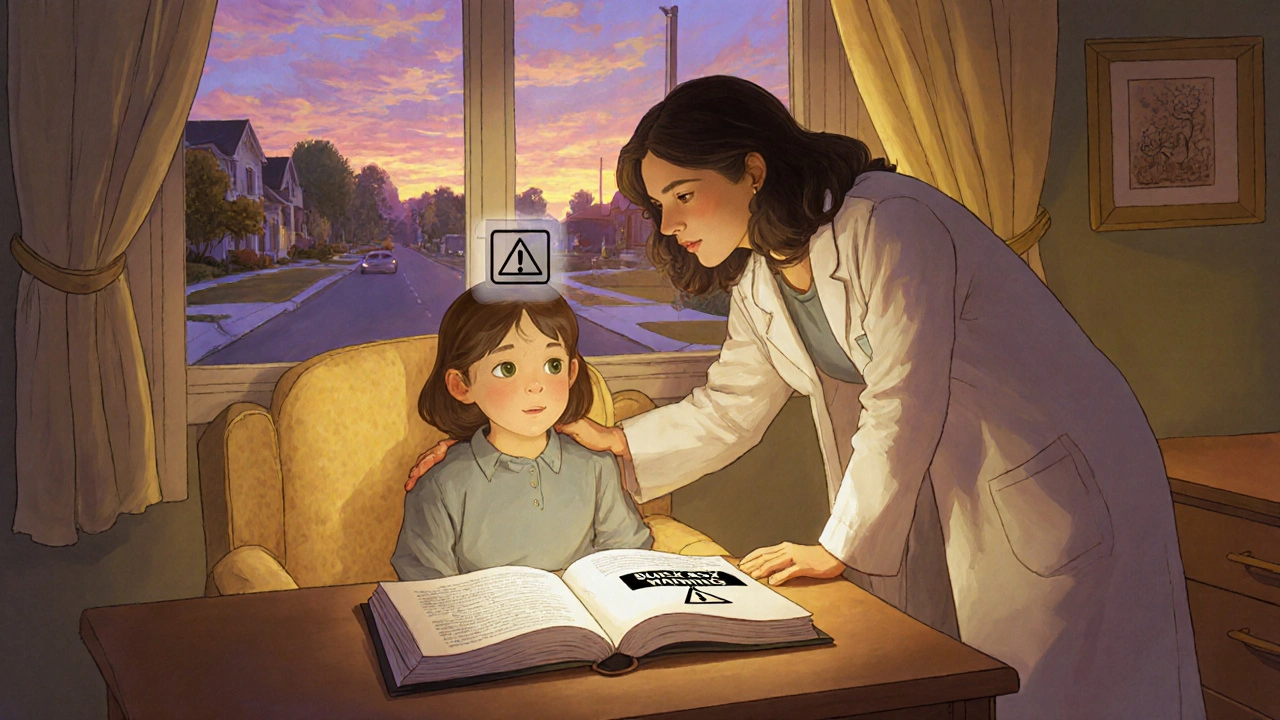
When a teenager shows signs of depression, the first question many parents ask is whether medication is safe. The answer isn’t simple, because the U.S. Food and Drug Administration (FDA) placed a Black Box Warning on every antidepressant for patients under 18 after data showed a higher chance of suicidal thoughts during the first months of treatment. This article unpacks what the warning really means, how clinicians should monitor young patients, and what the latest research says about risks and benefits.
What the FDA’s Black Box Warning actually says
Antidepressants are a class of drugs used to treat major depressive disorder (MDD), obsessive‑compulsive disorder (OCD) and several other psychiatric conditions. In October 2004, the FDA issued its most serious safety advisory - a Black Box Warning - after a pooled analysis of 24 clinical trials involving more than 4,400 pediatric participants. The analysis found that 4% of youths on antidepressants experienced suicidal thoughts or behaviors, compared with 2% on placebo, effectively doubling the relative risk. No actual suicides occurred in those trials, but the warning highlighted that the underlying disorders also carry a suicide risk.
The warning applies to all antidepressant classes, including selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine and sertraline, serotonin‑norepinephrine reuptake inhibitors (SNRIs) like venlafaxine, and atypical agents such as bupropion and mirtazapine. It mandates that manufacturers supply a Patient Medication Guide (MedGuide) outlining the risk and recommends close observation especially during the first few weeks and after any dose change.
Why the warning sparked controversy
Proponents point to the FDA’s 2004 data: a consistent pattern of increased suicidality across multiple drugs. Critics, however, argue that the warning caused a steep drop in antidepressant prescriptions, leading to unintended harms. A 2023 Health Affairs study showed a 22.3% reduction in antidepressant treatment among adolescents after the warning, accompanied by a 17.8% rise in completed suicides and a 21.7% increase in psychotropic drug poisonings - a proxy for suicide attempts.
Dr. Christine Y. Lu’s systematic review of 34 studies concluded that the warning may have done more harm than good, while other experts like Dr. Robert D. Gibbons argue that ecological studies linking prescription drops to suicide spikes are methodologically weak. The debate continues, and the FDA has kept the black‑box language unchanged as of October 2025.
Key monitoring recommendations from the warning
Regardless of the controversy, the warning sets clear monitoring expectations:
- Conduct a baseline suicide risk assessment before starting medication.
- Schedule weekly check‑ins (in‑person or telehealth) for the first month, then bi‑weekly for month two, and monthly thereafter.
- Use validated tools such as the Columbia‑Suicide Severity Rating Scale (C‑SSRS) at each visit.
- Document any worsening of depression, emergence of suicidal thoughts, or abrupt behavior changes.
- Communicate findings promptly to parents, schools, and any other involved caregivers.
The American Psychiatric Association’s 2022 practice guidelines echo these steps, emphasizing that monitoring should extend beyond the initial three‑month window if risk factors persist.
Comparing antidepressant classes in adolescents
Not all antidepressants carry the same profile of side effects or efficacy. Below is a quick snapshot of the most commonly prescribed classes for teens, based on data from CDC and IQVIA.
| Class | Typical First‑Line Drug | Suicidality Risk (Trial Avg.) | Prescription Share (2023) |
|---|---|---|---|
| SSRIs | Fluoxetine | 4% vs 2% placebo | 85% |
| SNRIs | Venlafaxine | ~5% vs 2% placebo | 9% |
| Atypical | Bupropion | 3% vs 2% placebo | 6% |
While the raw risk numbers appear similar, SSRIs remain the preferred first line because they have the most extensive safety data in youth and tend to be better tolerated.
Real‑world outcomes: what clinicians see in practice
A 2022 survey of 1,200 adolescent patients treated at the Mayo Clinic found that 87% reported symptom improvement without any suicidal ideation. About 3% experienced transient suicidal thoughts that resolved after a dose adjustment or a brief pause in treatment. These findings suggest that vigilant monitoring can keep the risk low for most teens.
Conversely, case reports published in Frontiers in Psychiatry illustrate the opposite extreme: two patients who declined medication after hearing about the Black Box Warning later attempted suicide, underscoring that avoidance can be dangerous.
Clinicians also report practical challenges. A 2021 Journal of the American Academy of Child & Adolescent Psychiatry survey showed that 76% of child psychiatrists experienced treatment delays averaging 3.2 weeks because families needed extra time to digest the warning. This delay can be crucial, as early intervention is associated with better long‑term outcomes.

Impact on prescribing patterns and public health
CDC data indicate that antidepressant prescriptions for youths aged 10‑19 fell 22.3% between 2004‑2006, reversing a previous upward trend. At the same time, suicide rates among the same age group rose 17.8% (2003‑2007). While correlation does not equal causation, the timing aligns with the warning’s rollout.
Industry monitoring from IQVIA shows that by 2023, prescription volumes remained about 18.7% below pre‑warning levels, despite a growing mental‑health burden highlighted by the Australian Bureau of Statistics and other international surveys.
Future directions: re‑evaluating the warning
Multiple professional bodies, including the American Academy of Child and Adolescent Psychiatry (AACAP) and the American Psychiatric Association, have formally petitioned the FDA to revisit the warning. A joint 2022 statement argued that for moderate‑to‑severe depression, the benefits of medication generally outweigh the risks.
Recent meta‑analyses add weight to the call for change. A 2023 Cochrane review of 34 randomized trials (6,772 participants) rated the evidence on suicidality as “low to very low,” noting sparse event rates and methodological gaps in the original studies. The FDA’s Psychopharmacologic Drugs Advisory Committee is slated to review the data in September 2024, and any amendment could shift how clinicians approach consent and monitoring.
Until policy changes occur, the best practice remains a balanced discussion: present the Black Box Warning transparently, outline the monitoring plan, and involve families in shared decision‑making.
Practical checklist for clinicians and families
- Before prescribing: Obtain a thorough psychiatric history, baseline C‑SSRS score, and discuss the Black Box Warning with the teen and caregivers.
- First month: Weekly visits or phone calls; reassess C‑SSRS; watch for mood swings, insomnia, or agitation.
- Months 2‑3: Bi‑weekly visits; adjust dose if side effects appear; continue risk assessment.
- Beyond 3 months: Monthly check‑ins; consider tapering only after stable remission for at least 6 weeks.
- Emergency plan: Provide 24‑hour crisis contacts, a written safety plan, and instructions for immediate care if suicidal thoughts intensify.
Following this framework can help keep the risk low while ensuring teens receive potentially life‑saving treatment.
What does the Black Box Warning say about suicide risk?
It alerts clinicians that children and adolescents have about twice the risk of suicidal thoughts or behaviors when starting an antidepressant, especially in the first few months of therapy.
Are all antidepressants equally risky for teens?
Risk levels are similar across classes, but SSRIs are preferred as first‑line agents because they have the most safety data and are better tolerated.
How often should a teen be monitored after starting an antidepressant?
Guidelines recommend weekly visits for the first month, then every two weeks for the second month, and monthly thereafter, using tools like the C‑SSRS each time.
Did the Black Box Warning reduce suicide rates?
Evidence is mixed. Some studies show a rise in suicide attempts after prescriptions fell, while others argue the warning’s benefit‑risk balance remains unclear.
Can the warning be removed or softened?
Professional societies have petitioned the FDA, and a 2024 advisory committee meeting may lead to revisions, but as of October 2025 the warning stays in place.

Miracle Zona Ikhlas
October 26, 2025 AT 17:27Monitoring teens closely in the first weeks can catch early warning signs and keep them safe.
naoki doe
November 8, 2025 AT 14:04The FDA’s pooled analysis of 4,400 pediatric participants revealed a 4% versus 2% incidence of suicidal thoughts on antidepressants versus placebo, effectively doubling the relative risk. That raw figure drives the recommendation for weekly check‑ins during the initiation phase.
Carolyn Cameron
November 21, 2025 AT 10:41It is incumbent upon the prescribing clinician to internalize the gravitas of the Black Box Warning, for it constitutes the pinnacle of regulatory admonition. The empirical substrate of this admonition rests upon a meta‑analytic conglomeration of randomized controlled trials wherein the incidence of suicidal ideation exhibited a statistically significant augmentation. Moreover, the temporal clustering of adverse events within the inaugural thirty days of therapy mandates a surveillance cadence that eclipses routine follow‑up. The confluence of pharmacodynamic variability and adolescent neurodevelopmental plasticity further exacerbates the potential for emergent suicidality. Consequently, a rigorous, protocol‑driven monitoring schema is not merely advisable but ethically obligatory.
Charlene Gabriel
December 4, 2025 AT 07:17When a family sits down to discuss the prospect of an antidepressant for their teenager, the conversation often begins with the ominous phrase “Black Box Warning.” That warning, while stark, is essentially a call to action for clinicians to implement a safety net that catches emerging distress before it escalates. The first step is a thorough baseline assessment, which should include not only a clinical interview but also standardized tools such as the C‑SSRS to quantify current suicidal ideation. Armed with that baseline, the prescriber can chart a visitation schedule that mirrors the heightened risk window-weekly contacts for the first four weeks, bi‑weekly for the subsequent month, and then monthly thereafter. Each encounter, whether in person or via telehealth, should revisit the assessment, probing for any shift in mood, sleep, appetite, or agitation that might herald worsening symptoms. Parents and caregivers play a pivotal role; they should receive a concise briefing on warning signs, such as sudden irritability, withdrawal, or uncharacteristic recklessness. Schools, too, can be enlisted as allies, with teachers alerted (with appropriate consent) to watch for concerning behavior changes during the academic day. Pharmacologically, the choice of agent matters; while SSRIs remain first‑line because of their extensive safety data, clinicians must remain vigilant for the idiosyncratic activation syndrome that occasionally surfaces with sertraline or fluoxetine. Should any suicidal thoughts emerge, the protocol dictates an immediate reassessment and, if needed, a temporary dose reduction or discontinuation, coupled with rapid referral to crisis services. It is also essential to document every interaction meticulously, noting the date, the C‑SSRS score, and any clinical observations, as this record becomes the backbone of medico‑legal protection. From a systems perspective, many practices have adopted electronic health record alerts that trigger reminders for upcoming check‑ins, reducing the likelihood of missed appointments. Insurance barriers can complicate this schedule, but many insurers now recognize the necessity of frequent monitoring for this high‑risk population and will reimburse telephonic or video visits. In the rare event that a teen experiences a severe adverse reaction, emergency services should be contacted without delay, and the family should be equipped with a written crisis plan that lists hotlines and local emergency department contacts. Research from the Mayo Clinic underscores that, when these safeguards are faithfully applied, the majority of adolescents-over eighty‑seven percent in one cohort-report symptomatic improvement without any suicidal ideation. Conversely, the literature also warns that omission of vigilant monitoring can transform a well‑intentioned prescription into a preventable tragedy, as illustrated by case reports of post‑prescription suicide attempts. Thus, the Black Box Warning is not a deterrent but a framework that, when integrated into collaborative care, can safeguard teens while granting them access to potentially life‑saving pharmacotherapy.
Leah Ackerson
December 17, 2025 AT 03:54One must ask whether we are treating symptoms or merely feeding a pharmaceutical treadmill; the moral calculus here is opaque 🤔. Yet the data compel us to respect the warning, lest we betray our duty to protect vulnerable youths 🛡️.
Gary Campbell
December 30, 2025 AT 00:31The FDA’s warning conveniently aligns with the profit motives of Big Pharma, which thrives on perpetual medication cycles; the real agenda is to keep teens dependent rather than cured.
renee granados
January 11, 2026 AT 21:07The warning is real, the risk is real, and ignoring it is reckless.
Stephen Lenzovich
January 24, 2026 AT 17:44Our nation’s mental health crisis cannot be solved by importing foreign drug regimens; we must demand homegrown solutions that respect American values and rigorous standards.
abidemi adekitan
February 6, 2026 AT 14:21Think of the monitoring plan as a lighthouse in a stormy sea, each beam of check‑in shining a safe path for the teen navigating the tumult of depression.
Barbara Ventura
February 19, 2026 AT 10:57Clearly, the Black Box Warning, while alarming, serves, in my view, as an essential, precautionary measure, demanding, without exception, heightened vigilance, systematic assessment, and unwavering parental involvement.