Antiviral Medication Interaction Checker
Check for Dangerous Interactions
Select your antiviral regimen and list other medications to see potential risks
Important: This tool is for educational purposes only. For medical advice, consult your healthcare provider. The University of Liverpool HIV Drug Interactions Checker is the gold standard for clinical use.
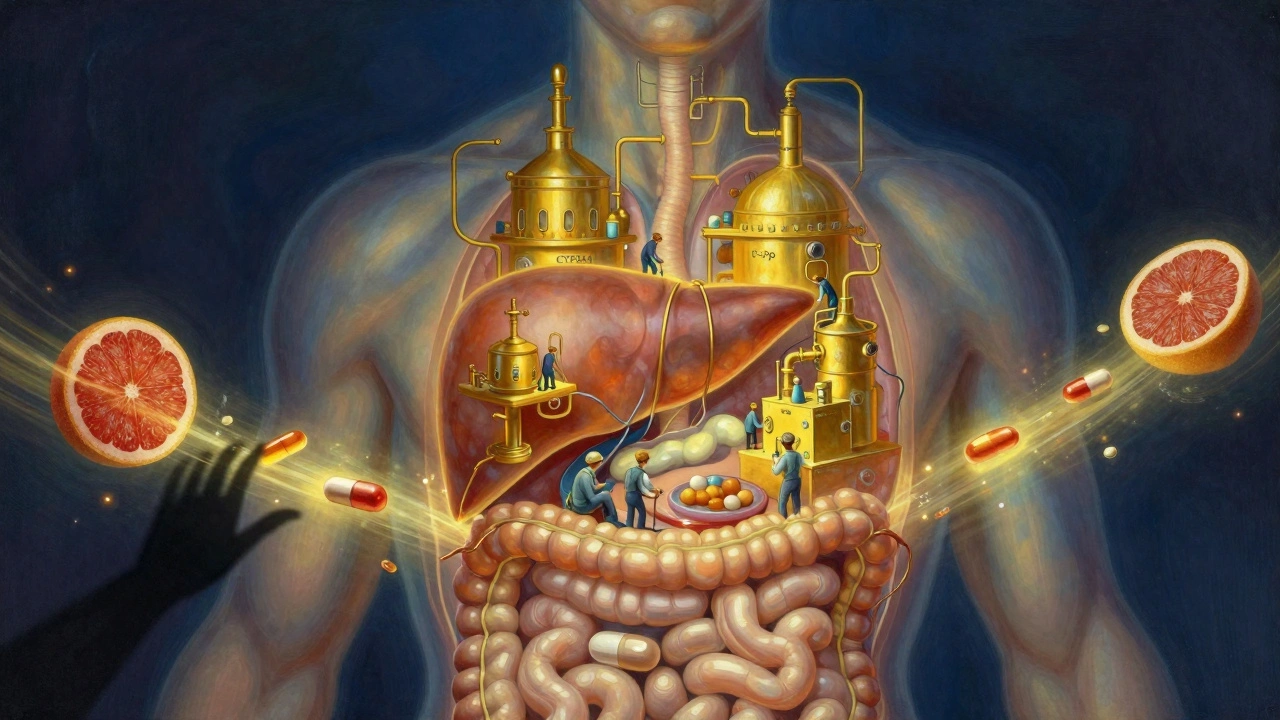
When you’re taking antiviral drugs for HIV or hepatitis C, it’s not just about the pill in your hand. What you’re really dealing with is a complex chemical dance inside your body - one that involves enzymes and transporters you’ve probably never heard of. Two of the biggest players? CYP3A4 and P-glycoprotein. These aren’t optional side notes. They’re make-or-break factors in whether your treatment works, causes side effects, or even lands you in the hospital.
What CYP3A4 and P-glycoprotein Actually Do
CYP3A4 is the most common enzyme in your liver and gut that breaks down drugs. Think of it like a recycling plant - it takes in medications and turns them into forms your body can flush out. About half of all prescription drugs pass through this system. Then there’s P-glycoprotein (P-gp), a molecular pump found in your intestines, liver, kidneys, and even the blood-brain barrier. Its job? To push drugs out before they can be absorbed or keep them from building up where they shouldn’t be.
When antivirals like ritonavir, darunavir, or glecaprevir enter your system, they don’t just go about their business. They interact with CYP3A4 and P-gp in one of three ways: as a substrate (something the enzyme or pump handles), an inhibitor (something that blocks the system), or an inducer (something that speeds it up). And here’s the catch - many antivirals do all three at once.
Ritonavir: The Original Game-Changer
Back in 1996, ritonavir was approved as an HIV protease inhibitor. But doctors quickly noticed something strange. When patients took it, other drugs - like lopinavir - stayed in their blood much longer. That wasn’t a side effect. It was a breakthrough.
Ritonavir turned out to be a powerful CYP3A4 inhibitor. At just 100 mg a day, it can boost the concentration of other antivirals by 300% to 500%. That’s why it became the go-to “booster” in drugs like Kaletra and many modern HIV regimens. But here’s the twist: ritonavir doesn’t just block CYP3A4. It also induces CYP1A2, another enzyme. That means it can simultaneously raise levels of some drugs while lowering others. For example, it can spike alprazolam (Xanax) levels by over 300% while cutting olanzapine (Zyprexa) levels by nearly 30%. This dual behavior makes it unpredictable - and dangerous - if you’re not careful.
How P-glycoprotein Makes Things Worse
Even if a drug survives CYP3A4, P-gp can still stop it from working. Many hepatitis C direct-acting antivirals (DAAs) like grazoprevir and paritaprevir are P-gp substrates. That means your body’s natural pump tries to shove them out before they can be absorbed. If you take something that blocks P-gp - like ritonavir - those antivirals get absorbed more easily. Sounds good? Not always.
That same boost can turn harmless drugs into toxic ones. Take digoxin, a heart medication. When taken with ritonavir, digoxin levels jump 2.8 times higher. That’s enough to cause dangerous heart rhythms. Same goes for apixaban (Eliquis), a blood thinner. A 2021 case report described a patient on apixaban who started darunavir/cobicistat and ended up with life-threatening bleeding because his anti-Xa levels soared to 384 ng/mL - way above the safe range of 50-250 ng/mL.

Comparing Antiviral Regimens: Who’s Safer?
Not all antivirals are created equal when it comes to interactions. Here’s how some common regimens stack up:
| Regimen | CYP3A4 Inhibition | P-gp Inhibition | Key Risk Drugs | Need for Dose Adjustments |
|---|---|---|---|---|
| Ritonavir-boosted (e.g., Kaletra) | Very Strong (AUC ↑ 11.3x) | Strong | Simvastatin, apixaban, warfarin | 42% |
| Cobicistat-boosted (e.g., Genvoya) | Strong (AUC ↑ 5.1x) | Strong | Simvastatin, colchicine, some antidepressants | 35% |
| Glecaprevir/pibrentasvir (Mavyret) | Mild | Mild | Most common meds safe | 17% |
| Sofosbuvir-based (e.g., Sovaldi) | Minimal | Modest | Warfarin, statins (mostly safe) | 10% |
| Darunavir (unboosted) | Very Weak (AUC ↑ 1.2x) | None | Mostly safe | 5% |
Notice the pattern? The older, boosted regimens - especially those with ritonavir - are interaction magnets. Newer drugs like Mavyret and unboosted darunavir are much cleaner. But even “clean” drugs aren’t risk-free. Sofosbuvir doesn’t touch CYP3A4, but it’s still affected by P-gp. And if you’re on multiple meds for diabetes, high blood pressure, or depression, you’re still in danger.
What You’re Not Being Told: The Hidden Risks
Most doctors focus on CYP3A4. But that’s only half the story. A 2022 study in Antimicrobial Agents and Chemotherapy found that 22% of serious drug interactions were caused by other transporters - like OATP1B1 and BCRP - that barely get mentioned in guidelines.
Take cyclosporine, a transplant drug. When taken with grazoprevir (part of Mavyret), it causes a 17.3-fold spike in blood levels. That’s not a typo. That’s a recipe for kidney failure. The European Association for the Study of the Liver lists this as a Level 4 - contraindicated - interaction. Yet, many patients on antivirals are also on statins, blood thinners, or immunosuppressants. No one asks about them.
And then there’s the herbal stuff. St. John’s wort? It can slash ritonavir levels by 57%. Grapefruit juice? It can bump them up by 23%. Both are common. Both are dangerous. Most patients don’t think of them as “medications,” but they’re just as powerful as pills.
Real Stories, Real Consequences
One patient in a 2021 case report took apixaban for atrial fibrillation. After starting darunavir/cobicistat, he had major internal bleeding. His blood thinner levels were off the charts. He survived - barely.
Another patient, a 68-year-old on warfarin, was prescribed a ritonavir-boosted HIV regimen. His INR (a measure of blood clotting) shot up so high he needed hospitalization. Four out of twelve similar cases in one 2021 study ended the same way.
On the flip side, clinics using the University of Liverpool HIV Drug Interactions Checker saw interaction-related hospitalizations drop from 18.7% to 5.2% in just one year. That app isn’t fancy. It doesn’t need a prescription. It’s free. And it’s used by over 1.2 million people worldwide.
What You Should Do Right Now
If you’re on an antiviral - especially for HIV or hepatitis C - here’s your action list:
- Make a full list of everything you take: prescriptions, OTC meds, vitamins, supplements, and herbal products. Don’t leave anything out.
- Use the Liverpool HIV Interactions Checker (free online or as an app). Enter every drug you’re taking. It will flag risks in red, yellow, or green.
- Ask your pharmacist to run a drug interaction screen. Pharmacists are trained for this. Most won’t do it unless you ask.
- Don’t start new meds - even for anxiety or sleep - without checking. One Reddit user said his psychiatrist refused to prescribe anything because of his HIV meds. He wasn’t being denied care. He was being protected.
- Check for timing. Some interactions are worse at first. Delaying a blood thinner by a month after starting an antiviral can avoid dangerous peaks.
The Bigger Picture
By 2025, 39 million people worldwide will be on antiretroviral therapy. Most are over 50. Most have other conditions: diabetes, heart disease, depression, arthritis. That means more meds. More interactions. More risk.
Drugmakers are catching on. New antivirals like lenacapavir are being designed to avoid CYP3A4 and P-gp entirely. But until then, the old ones are still everywhere. And they’re still dangerous if you don’t know how to handle them.
Antiviral treatment isn’t just about killing the virus. It’s about keeping the rest of your body safe. The science is clear. The tools exist. The question is: are you using them?
Can I take grapefruit juice with my antiviral medication?
No. Grapefruit juice contains bergamottin, which inhibits CYP3A4 in your gut. This can cause your antiviral - especially ritonavir or cobicistat - to build up to toxic levels. Even one glass can raise drug concentrations by 23%. Avoid it completely while on these medications.
Is there a safer antiviral with fewer drug interactions?
Yes. Glecaprevir/pibrentasvir (Mavyret) and unboosted darunavir have far fewer interactions than ritonavir- or cobicistat-boosted regimens. Mavyret only requires dose adjustments for 17% of common medications, compared to 42% for older combinations. If you’re starting treatment, ask your doctor if a low-interaction option is right for you.
Why does my doctor keep asking about my other medications?
Because antivirals like ritonavir and cobicistat can dangerously increase or decrease levels of other drugs - including blood thinners, statins, antidepressants, and even over-the-counter painkillers. A 2021 study found that 17.3% of adverse events in HIV/hepatitis C patients were due to unrecognized drug interactions. Your doctor isn’t being overly cautious - they’re preventing a life-threatening reaction.
Can I use St. John’s wort for depression while on antivirals?
Absolutely not. St. John’s wort induces CYP3A4 and can reduce ritonavir levels by up to 57%. That means your HIV treatment could fail, leading to drug resistance. Even if you feel fine, you’re risking long-term damage. Always tell your doctor about herbal supplements - they’re not harmless.
How do I know if my antiviral is boosting another drug?
If your antiviral regimen includes the word “boosted” - like darunavir/ritonavir or elvitegravir/cobicistat - then yes, one drug is boosting another. Ritonavir and cobicistat are never used alone. They’re there to slow down how fast your body breaks down the main antiviral. That’s why they’re so powerful - and so risky.
Should I get genetic testing before starting antivirals?
It’s not routine yet, but it’s becoming more useful. People with the CYP3A5*3/*3 genotype (common in Caucasians) break down certain drugs much slower. When combined with ritonavir, this can lead to 2.3 times higher exposure to drugs like tacrolimus. If you’re on multiple medications or have a history of side effects, ask your doctor if pharmacogenomic testing is right for you.
What’s the best tool to check for drug interactions?
The University of Liverpool HIV Drug Interactions Checker is the gold standard. It’s free, updated weekly, and used by clinics worldwide. It gives color-coded warnings (red = dangerous, yellow = caution, green = safe) and includes details on OATP and P-gp interactions - something most apps miss. Download the app or use it online at hiv-druginteractions.org.
Next Steps: What to Do Today
If you’re on antivirals, don’t wait. Right now, open your medicine cabinet. Write down every pill, capsule, and supplement. Then go to hiv-druginteractions.org. Enter each one. If anything shows red, call your doctor or pharmacist before taking another dose. Don’t assume they know. Don’t assume it’s safe. This isn’t theoretical - it’s life-or-death.

Richard Eite
December 8, 2025 AT 16:20Philippa Barraclough
December 9, 2025 AT 14:49Tim Tinh
December 11, 2025 AT 09:55Jennifer Blandford
December 11, 2025 AT 20:55Brianna Black
December 12, 2025 AT 10:09Shubham Mathur
December 12, 2025 AT 12:30Stacy Tolbert
December 14, 2025 AT 10:49Ronald Ezamaru
December 16, 2025 AT 04:27Gilbert Lacasandile
December 16, 2025 AT 12:01Lola Bchoudi
December 18, 2025 AT 08:07Morgan Tait
December 19, 2025 AT 03:47om guru
December 20, 2025 AT 09:51Ryan Brady
December 21, 2025 AT 22:44