Ataxia isn't a single disease. It's a symptom - a loss of coordination that makes walking, talking, and even holding a cup feel impossible. People with ataxia don't just feel clumsy. Their body doesn't respond the way it should. One moment they're standing, the next they're falling. Words come out slurred. Eyes jump uncontrollably. It's not weakness. It's not laziness. It's the brain's motor control system breaking down, usually because the cerebellum - the part of the brain that fine-tunes movement - is damaged.
What Causes Ataxia?
There are three main types of ataxia, each with different causes and progression patterns. Hereditary ataxias are passed down through genes. Friedreich's ataxia is the most common, often starting in childhood or teens. People with this form slowly lose the ability to walk, and many develop heart problems or diabetes. There are over 45 types of spinocerebellar ataxia, each caused by a different gene mutation. These usually appear between ages 20 and 50 and get worse over time.Acquired ataxia happens suddenly. It's often triggered by something external: a stroke, a head injury, an infection like Lyme disease or HIV, or even a vitamin B12 deficiency. In these cases, if the root cause is caught early and treated - say, by giving B12 shots or clearing a brain clot - coordination can improve or even fully return.
Then there's idiopathic late-onset cerebellar ataxia (ILOCA). This one shows up after age 50 with no clear cause. No genetic link. No known injury. Just a slow, steady decline in balance and movement. It's frustrating because doctors can't point to why it's happening, only how to manage it.
How Ataxia Changes Your Body
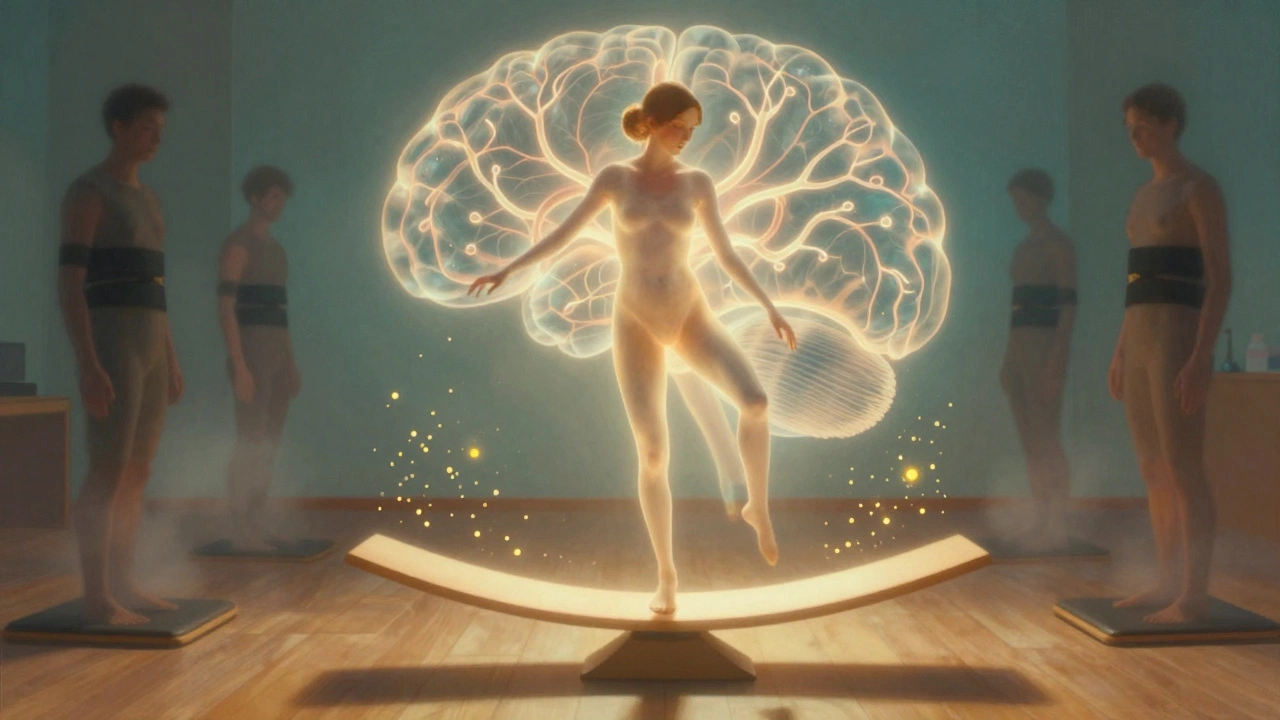
The cerebellum has about 69 billion neurons - more than the rest of the brain combined. When it's damaged, the timing of your movements goes off. Your brain sends the signal to move your arm, but the signal arrives too late, too early, or too strong. That's why you knock over your coffee, stumble on flat ground, or can't write your name clearly.Nearly everyone with ataxia has trouble walking. Studies show 98% of patients struggle with gait stability. About 92% have dysarthria - speech that sounds drunk or mumbled. And 85% experience abnormal eye movements, making it hard to focus on a face or read a screen. These aren't minor inconveniences. They turn everyday tasks into high-risk activities. Getting out of a chair. Pouring water. Buttoning a shirt. All become potential fall hazards.
It's not just physical. Around 70% of people with ataxia also deal with cognitive changes - trouble planning, remembering instructions, or staying focused. This makes rehab harder. If you can't remember the exercise routine your therapist gave you, progress stalls.
Neurological Rehabilitation: The Only Real Treatment
There are no drugs that cure most types of ataxia. The 2022 American Academy of Neurology guidelines are clear: no disease-modifying therapies exist. That means rehab isn't optional - it's the core of treatment.Traditional physical therapy often fails people with ataxia. Generic balance exercises or strength training won't fix the timing problem in the brain. What works is task-specific training. This means practicing real-life movements over and over, with precision. Not just standing on one foot. Standing on one foot while catching a ball. Walking while counting backward. Reaching for a cup while turning your head.
Studies show this approach leads to 35% better results than standard PT. A 2021 Mayo Clinic trial found patients using computerized balance systems like the NeuroCom SMART Balance Master improved their balance scores by 8.2 points on average - nearly double the gain from regular therapy. The key? Real-time feedback. Sensors tell you exactly how much you're swaying, so your brain learns to correct itself.
But not all rehab tools work. Robotics that help stroke patients walk again? They barely help ataxia. Constraint-induced therapy, which forces use of a weak limb? It makes ataxia worse in 68% of cases. The problem? Ataxia isn't about muscle weakness. It's about faulty brain signals. You can't force a broken clock to tick right by pushing its hands.

What Does a Real Ataxia Rehab Program Look Like?
Effective rehab follows a clear structure. The 2022 International Ataxia Rehabilitation Guidelines break it into three phases:- Phase 1 (Weeks 1-4): Static balance. Standing still with eyes open, then closed. Adding dual tasks - like talking while standing. This trains the brain to multitask without losing control.
- Phase 2 (Weeks 5-8): Dynamic movement. Walking on uneven surfaces, stepping over obstacles, turning quickly. This builds confidence in motion.
- Phase 3 (Weeks 9-12): Real-world skills. Walking in a store, going up stairs, getting in and out of a car. Fall prevention becomes the goal.
Each session lasts 60 to 90 minutes, 3 to 5 times a week. It's intense. 89% of patients report extreme fatigue. But the payoff? A 2021 Cochrane review of 37 studies found that people who stuck with this level of rehab improved their functional independence by 25-40%. That means more meals eaten alone, fewer falls, less reliance on caregivers.
Technology Is Changing the Game - But Not Everyone Can Access It
New tools are making rehab more precise. Wearable sensors like the APDM Opal track 17 different gait parameters - step length, speed, symmetry - and give therapists data they never had before. Virtual reality systems like CAREN create immersive environments where patients practice walking through busy streets or across bridges, all in a safe clinic setting. One study showed 28% higher engagement with VR than traditional therapy.Then there's the Cerebello wearable, FDA-cleared in 2023. It uses targeted neuromodulation to reduce tremors in the hands. In trials, users improved upper limb function by 32%. That’s huge for someone who can't hold a spoon.
But here's the problem: these tools cost $120,000 to $350,000 per system. Only 15% of rehab centers in the U.S. have them. Most patients get basic balance pads and resistance bands. And even those aren't always delivered by trained staff.
There are only 327 physical therapists in the U.S. certified in the CRED (Cerebellar Rehabilitation and Evaluation Dynamics) program - a 120-hour specialized training. In rural areas, that's one therapist for every 458 patients. In cities, it's one per 87. If your therapist doesn't know ataxia, they might prescribe exercises that make things worse.

Real People, Real Struggles
Patient stories tell the real story. One Reddit user, 'AtaxiaWarrior87,' spent eight months with generic PT that left them worse. Then they found a CRED-certified therapist. In 10 weeks, their SARA score - a standard ataxia severity scale - dropped from 18 to 12. That's not just numbers. That's being able to walk to the mailbox again.But many can't afford it. Insurance often caps rehab at 20 visits, no matter what the doctor says. One patient paid $3,200 out-of-pocket after their insurance cut off coverage. Medicare and private insurers cover about 65% of costs, but out-of-pocket expenses still average $2,450 a year. For someone earning under $50,000 - 31% of ataxia patients - that’s a huge burden.
Home programs help. 68% of people who stick with daily exercises at home see measurable gains. Aquatic therapy, done in a pool, is rated 4.3 out of 5 for effectiveness. The water supports your body, letting you move without fear of falling. Telehealth is another lifeline, especially for rural patients. 70% of those using virtual rehab report satisfaction.
The Future Is Here - But Only for Some
Research is moving fast. A 2024 study in Brain Stimulation found that combining transcranial direct current stimulation (ctDCS) - a mild electric pulse to the cerebellum - with physical therapy boosted improvement by 22% over therapy alone. A major NIH-funded trial (NCT05112345) is testing whether intensive rehab over 6 weeks beats spread-out sessions. Results come in late 2025.But big gaps remain. There's no test to predict who will respond to rehab. Doctors guess. Patients wait 6-12 months before getting the right treatment. And globally, there's a shortage of 1.2 million neurorehab professionals. Ataxia expertise? Even rarer.
Without policy changes - like lifting visit limits, expanding CRED training, and funding home tech - 65% of ataxia patients will lose access to effective care by 2030. The tools exist. The science is solid. But the system isn't keeping up.
What You Can Do
If you or someone you love has ataxia:- Ask your neurologist for a referral to a therapist with ataxia-specific training. Look for CRED certification.
- Insist on using the SARA scale to track progress. If your clinic doesn't use it, ask why.
- Push for home exercises. Even 20 minutes a day helps.
- Explore telehealth. It's often covered, even if in-person visits aren't.
- Join a patient community. Reddit's r/ataxia and the National Ataxia Foundation offer real advice from people living it.
Ataxia doesn't have a cure. But with the right rehab, it doesn't have to take your life either. Progress is slow. It's hard. But it's possible. And every step forward - even a small one - is worth fighting for.
Can ataxia be cured?
There is no cure for most types of ataxia, especially hereditary forms. However, acquired ataxia - caused by things like vitamin deficiency, infection, or stroke - can sometimes be reversed if the underlying cause is treated quickly. For all types, neurological rehabilitation is the most effective way to improve function and quality of life.
How long does ataxia rehabilitation take to show results?
Most people start seeing small improvements in balance and coordination within 4-6 weeks of intensive therapy. Significant gains - like walking without assistance or reducing falls - typically take 8-12 weeks of consistent, task-specific training. Progress continues with ongoing therapy, but it's gradual. Patience and consistency are key.
Is physical therapy the only option for ataxia rehab?
No. A full rehab program includes physical therapy, occupational therapy (to help with daily tasks like dressing and eating), and speech-language pathology (for slurred speech). Aquatic therapy, virtual reality, wearable tech, and home exercise programs are also effective. The best approach combines all these elements tailored to the individual's needs.
Why do some therapists make ataxia worse?
Many therapists are trained for stroke or spinal cord injuries, not cerebellar disorders. Techniques like constraint-induced movement therapy - which forces use of a weak limb - can overwhelm the brain's already impaired timing system in ataxia. This leads to increased unsteadiness and falls. Always ask if your therapist has specific training in ataxia rehabilitation.
Can I do ataxia rehab at home?
Yes - and it's essential. Home exercises reinforce what you learn in therapy. Simple routines like standing on one foot while holding a chair, walking heel-to-toe, or practicing reaching for objects while turning your head can make a big difference. Use mirrors for feedback. Record yourself. Stay consistent. Studies show 68% of people who stick to home programs see measurable improvement.
Does insurance cover ataxia rehabilitation?
Most insurance plans cover medically necessary rehab, but often with strict limits - like 20 visits per year - regardless of progress. Medicare typically covers 65% of costs, but out-of-pocket expenses average $2,450 annually. Many patients face denials or require appeals. Always get a doctor's note stating medical necessity and keep detailed records of your symptoms and progress.
What's the difference between ataxia and Parkinson's?
Ataxia is caused by damage to the cerebellum and results in uncoordinated, clumsy movements - like stumbling, slurred speech, and jerky eye movements. Parkinson's affects the basal ganglia and causes tremors at rest, stiffness, slow movement, and a shuffling gait. While both affect movement, the underlying brain areas, symptoms, and rehab approaches are very different.

Shannara Jenkins
December 3, 2025 AT 07:10Just wanted to say thank you for writing this. My mom was diagnosed with ILOCA last year, and this is the first time I’ve seen someone explain it so clearly. We’ve been struggling to find a therapist who even knows what ataxia is. Now I know to ask for CRED certification. 💛
Zed theMartian
December 3, 2025 AT 11:21Oh please. ‘Task-specific training’? That’s just rehab theater. You’re telling me 69 billion neurons in the cerebellum can be ‘retrained’ like a dog with treats? This is pseudoscience dressed up in clinical jargon. If you want real progress, try transcranial magnetic stimulation - not some fancy balance pad from 2021.
Ella van Rij
December 4, 2025 AT 01:54Wow. So much text. So many numbers. So little actual science. I mean, ‘89% report extreme fatigue’ - wow, shocker. Next you’ll tell me breathing is hard when you’re falling over. Also, ‘CRED certification’? Sounds like a LinkedIn badge you buy after a weekend webinar.
ATUL BHARDWAJ
December 4, 2025 AT 11:58In India, we have no access to these machines. But my cousin, he walks with stick, does daily heel-to-toe on floor. Now he can feed himself. No tech. Just will. Simple things matter more than fancy gadgets.
Steve World Shopping
December 6, 2025 AT 05:55Let me be blunt: the entire rehabilitation paradigm is fundamentally misaligned with the neurophysiological reality of cerebellar dysfunction. The reliance on behavioral conditioning without neuroplasticity modulation is not just inefficient - it’s epistemologically bankrupt. You need neuromodulatory interventions, not balance pads. Period.
Rebecca M.
December 7, 2025 AT 23:06So let me get this straight… you spent 120 hours learning how to help people not fall down… and insurance only pays for 20 visits? And you’re surprised people are angry? Honey, this isn’t rehab. It’s a hostage situation with a physical therapist holding the keys to dignity.
Lynn Steiner
December 9, 2025 AT 02:34I’ve been doing this for 7 years. I’ve lost my job. My husband left. I can’t hug my kids without falling. And you want me to do 90-minute sessions 5x a week? I’m tired. I’m broke. And I’m so sick of people saying ‘just stay consistent.’ Consistent with what? With being broken?
😭
Alicia Marks
December 10, 2025 AT 18:58You got this. Even 10 minutes a day counts. You’re not failing - you’re fighting. And that’s more than most people ever do.
Paul Keller
December 11, 2025 AT 03:21While the article presents a compelling and largely evidence-based overview of ataxia rehabilitation, it is critically deficient in addressing the socioeconomic determinants of care access. The disparity between urban and rural therapist availability - 1:87 versus 1:458 - is not merely a logistical issue; it is a systemic failure of healthcare policy. Furthermore, the exclusion of non-Western rehabilitation models, such as Ayurvedic balance therapies or community-based mobility training in low-resource settings, renders the discussion culturally myopic. The assertion that ‘the tools exist’ is misleading without acknowledging that access is not a function of availability, but of equity.
Elizabeth Grace
December 12, 2025 AT 23:34I just got my first Cerebello wearable last month. I cried the first time I held a spoon without shaking. It’s not magic. But after 5 years of falling, it’s the first thing that didn’t make me feel like a broken toy. Thank you for not pretending this is just about ‘exercise’.