When you’re over 65 and taking medicine for high blood pressure, standing up too fast can make you dizzy-or worse, cause a fall. This isn’t just a minor inconvenience. It’s a real danger, and it’s more common than most people realize. About one in five older adults on blood pressure meds experience orthostatic hypotension: a sudden drop in blood pressure when standing. The irony? The very drugs meant to protect your heart can sometimes put you at risk for injury. But here’s the twist: taking less medicine isn’t always the answer. In fact, doing the opposite might be safer.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension happens when your blood pressure drops by at least 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure within three minutes of standing. Your body normally adjusts quickly-blood vessels tighten, heart rate increases-to keep blood flowing to your brain. But as you age, that system slows down. Baroreceptors (your body’s pressure sensors) don’t respond as fast. Blood volume drops. Blood vessels stiffen. Your heart doesn’t pump as efficiently. All of this makes standing up feel like stepping off a cliff. For seniors with high blood pressure, this isn’t random. It’s a side effect tied to specific medications. The problem isn’t just dizziness. It’s falls. Falls lead to fractures, hospital stays, and loss of independence. And yet, many doctors still assume that lowering blood pressure too much causes this. That assumption is outdated-and dangerous.Which Blood Pressure Meds Carry the Highest Risk?
Not all blood pressure drugs are created equal when it comes to orthostatic risk. Some are much safer than others, especially for older adults.- Alpha blockers (like doxazosin, terazosin) have the highest risk-up to 28% of older patients on these meds develop orthostatic hypotension. They relax blood vessels too aggressively, especially when standing.
- Beta-blockers (like metoprolol, atenolol) carry a 3.36 times higher risk of sustained low blood pressure upon standing. They slow the heart’s ability to compensate.
- Diuretics (like hydrochlorothiazide) reduce fluid volume, which can make blood pressure drop too low when upright.
- Central sympatholytics (like clonidine) interfere with the nervous system’s natural response to standing.
On the flip side, some medications are actually safer-or even protective:
- ACE inhibitors (like lisinopril) and ARBs (like losartan) show the lowest risk. Studies show they reduce orthostatic hypotension episodes by 14-15% compared to other classes. They don’t over-dilate vessels or blunt heart rate responses.
- Amlodipine and isradipine (calcium channel blockers) are better tolerated than older versions like diltiazem or verapamil. Their slow action means less sudden drops in pressure.
Here’s what the data says: if you’re on an alpha blocker or a beta-blocker and you’re dizzy when you stand, switching to an ARB or ACE inhibitor could cut your fall risk by up to 65%-without sacrificing blood pressure control.
More Aggressive Treatment? Yes-But Only With the Right Drugs
For years, doctors feared that pushing systolic blood pressure below 130 mm Hg would cause dangerous drops when standing. The SPRINT trial shattered that myth. In a study of over 9,000 adults over 50 with high blood pressure, those targeted to a systolic pressure of less than 120 mm Hg didn’t have more orthostatic hypotension than those targeting 140 mm Hg. In fact, the intensive group had a 17% lower risk of developing it. Why? Because when you use the right drugs-like ARBs and ACE inhibitors-you’re not just lowering pressure. You’re improving how your body manages it. Aggressive treatment with safe medications reduces strain on the heart and arteries, which helps your body adapt better to position changes. The takeaway? Don’t lower your blood pressure goals just because you’re dizzy. Lower your risk by changing your meds, not your target.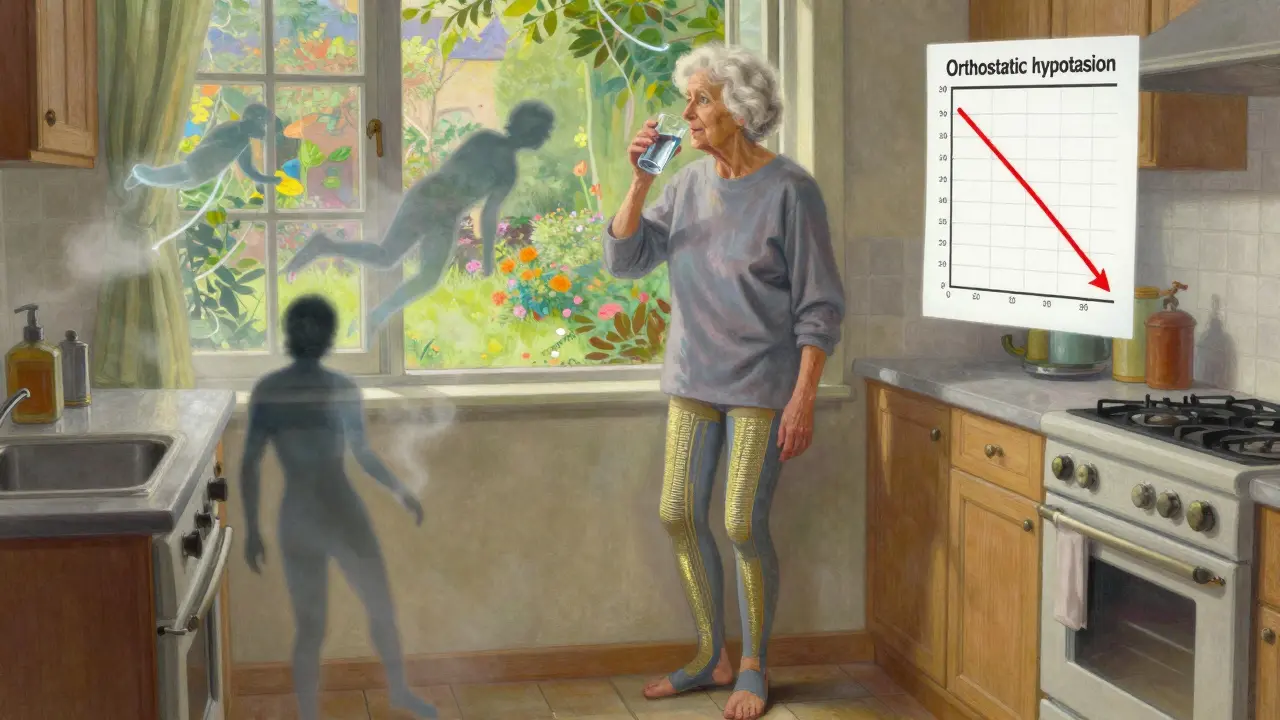
Non-Medication Strategies That Actually Work
Before you even think about switching pills, try these simple, proven steps. They cost nothing, have no side effects, and work for most people within weeks.- Stand up slowly. Sit on the edge of the bed for 30 seconds before standing. Pause again at the sink before walking.
- Hydrate before rising. Drink 16 oz of water 15 minutes before getting up. It boosts blood volume and helps maintain pressure.
- Avoid large meals. Blood flows to your gut after eating, which can drop pressure. Eat smaller meals more often.
- Wear compression stockings. They help push blood back up from your legs. Studies show they reduce dizziness by 40% in older adults.
- Don’t stand still for long. If you’re waiting in line, shift your weight or march in place.
Many patients report feeling better within 2-4 weeks of consistently practicing these habits. No pills needed.
When Medication Is Still Needed
Sometimes, lifestyle changes aren’t enough. If you’re still fainting or falling despite these steps, your doctor may consider adding a drug specifically for orthostatic hypotension. These aren’t first-line-they’re rescue options.- Midodrine tightens blood vessels in the legs and abdomen. It’s taken 3 times a day, but never after 6 p.m.-it can cause high blood pressure while lying down.
- Droxidopa helps your body make norepinephrine, which raises standing pressure. Used for neurogenic orthostatic hypotension.
- Fludrocortisone increases salt and water retention. Risky in people with heart failure.
- Pyridostigmine boosts nerve signals to blood vessels. Less commonly used but helpful in some cases.
These drugs have side effects. Midodrine can cause scalp tingling or supine hypertension. Droxidopa may cause headaches. Always monitor blood pressure lying down when using them.
What to Ask Your Doctor
If you’re over 65 and on blood pressure meds, here are five questions to ask at your next visit:- Could any of my current medications be causing my dizziness when I stand?
- Would switching to an ARB or ACE inhibitor reduce my risk of orthostatic hypotension?
- Am I on too many blood pressure drugs? Could one be stopped safely?
- Have you checked my blood pressure both lying down and standing up?
- Can we review all my meds-including supplements and over-the-counter drugs? Some (like NSAIDs or sleep aids) make OH worse.
Don’t assume dizziness is just "part of aging." It’s a warning sign-and it’s fixable.
The Bigger Picture: Why This Matters
In the U.S., over 74 million adults over 65 have high blood pressure. Of those, an estimated 2.2 to 19.4 million also have orthostatic hypotension. That’s millions of people at risk for falls, fractures, and hospitalization. The good news? We now know how to prevent it. The American Geriatrics Society Beers Criteria updated its guidelines in 2023 to flag alpha blockers and certain beta-blockers as potentially inappropriate for seniors with OH risk. More doctors are catching on. Prescriptions for ARBs and ACE inhibitors in seniors rose from 32% in 2020 to 38% in 2023-not because they’re cheaper, but because they’re smarter. The future is even brighter. Researchers are testing "smart" blood pressure drugs that only activate when you stand up. Two are already in Phase II trials. In five years, personalized treatment plans that check for orthostatic risk before prescribing may become standard.Bottom Line: Safety Isn’t About Less Medicine-It’s About Better Medicine
You don’t need to choose between protecting your heart and staying steady on your feet. You just need the right combination of drugs and habits. Stop assuming dizziness means you’re taking too much. Ask if you’re taking the right kind. Switch from high-risk meds like alpha blockers to safer ones like ARBs. Practice standing slowly. Drink water before rising. Wear compression socks. These aren’t just tips. They’re evidence-backed tools that can keep you independent, mobile, and safe. And that’s what really matters when you’re aging with high blood pressure.Can blood pressure medication cause dizziness when standing?
Yes, certain blood pressure medications-especially alpha blockers, beta-blockers, diuretics, and central sympatholytics-can cause orthostatic hypotension, which leads to dizziness, lightheadedness, or fainting when standing up. This happens because these drugs lower blood pressure too quickly or interfere with the body’s natural ability to adjust to posture changes. Not all blood pressure meds cause this, though. ACE inhibitors and ARBs are much safer and may even reduce the risk.
Should I stop my blood pressure medicine if I feel dizzy?
No. Stopping your medication without medical guidance can raise your blood pressure dangerously and increase your risk of stroke or heart attack. Instead, talk to your doctor. Dizziness may mean you’re on a high-risk drug that can be swapped for a safer one-not that you need less medicine. Studies show that aggressive blood pressure control with the right drugs actually reduces orthostatic hypotension risk.
What’s the safest blood pressure medicine for seniors?
ACE inhibitors (like lisinopril) and ARBs (like losartan) are the safest options for seniors at risk of orthostatic hypotension. They have the lowest incidence of causing dizziness upon standing-around 8-10%-and may even help prevent it. Among calcium channel blockers, amlodipine and isradipine are preferred over diltiazem or verapamil due to their slower, gentler action on blood vessels.
How long does it take to adjust to new blood pressure meds?
It usually takes 4 to 6 weeks for your body to fully adjust to a new blood pressure medication, especially when switching from a high-risk drug to a safer one. During this time, your doctor should monitor your blood pressure both lying down and standing. Non-medication strategies like slow standing and hydration often show improvement within 2-4 weeks.
Can drinking more water help with dizziness from blood pressure meds?
Yes. Drinking 16 ounces of water 15 minutes before standing can boost blood volume and help prevent sudden drops in pressure. This is especially helpful after waking up, after meals, or after using the bathroom. Hydration is one of the most effective, low-cost, side-effect-free ways to reduce orthostatic dizziness in older adults.


John Chapman
January 1, 2026 AT 02:14OMG THIS IS LIFE-SAVING INFO!!! 🙌 I was on doxazosin for years and thought my dizziness was just "getting old"-switched to losartan and now I can stand up without feeling like I’m gonna faint. My grandkids finally stopped asking if I’m okay every time I get up from the couch. THANK YOU for this post!!! 💪❤️
Urvi Patel
January 1, 2026 AT 23:04Most doctors still treat seniors like broken machines that need less medicine not better ones. This is why healthcare in the US is a joke. The real problem is lazy prescribing and no follow up. ARBs are not magic they’re just less destructive. Still too many people die because someone didn’t bother to check standing BP. Basic stuff. Basic.
anggit marga
January 2, 2026 AT 05:33Y’all in the US overthink everything. In Nigeria we just tell grandmas to stand slow and drink more water. No fancy pills. No doctor visits. No insurance headaches. You think your meds are safe? My uncle took amlodipine and still fell. Now he uses a cane. Maybe the problem isn’t the drug maybe it’s the whole system pretending it knows what it’s doing.
Joy Nickles
January 3, 2026 AT 10:06Wait wait wait-so you’re saying I shouldn’t just stop my metoprolol because I get dizzy?? But my friend’s cousin’s neighbor’s aunt said she stopped hers and her BP went from 180 to 120 in two days?? And now she’s running marathons?? I’m confused. Also I think I’m allergic to the word ARB. Can I just drink more coffee instead?? 😅
Emma Hooper
January 4, 2026 AT 23:26Let me be the first to say this out loud: your doctor isn’t your enemy-but they’re probably overworked, underpaid, and didn’t get enough training on geriatric pharmacology. The fact that alpha blockers are still prescribed to seniors like they’re harmless? That’s not negligence. That’s systemic laziness. And yet here we are. You’re not crazy for feeling dizzy. You’re just the victim of outdated guidelines and a profit-driven system that rewards volume over wisdom. This post? It’s a middle finger to medical complacency. Keep fighting.
Marilyn Ferrera
January 5, 2026 AT 13:49Hydration before standing. Slow movements. Compression socks. These are not "hacks." They are physiological necessities. The body isn’t broken. It’s being ignored. And yes, ARBs are safer. But only if you take them as directed. And if your doctor won’t check your orthostatic BP? Find a new one. Your independence is worth it.
linda permata sari
January 7, 2026 AT 02:59When I was in Jakarta, my abuela drank ginger tea every morning and stood up like a queen. No meds. No stress. Just slow breaths and gratitude. You think science is the only answer? Maybe it’s also about culture. About respect. About honoring the body’s rhythm. We lost that. And now we’re paying with fractures and fear.
Brandon Boyd
January 7, 2026 AT 10:26I’ve been telling my mom for years to switch from atenolol to lisinopril. She didn’t listen until she fell and broke her hip. Now she’s on ARBs, drinks water like it’s her job, and wears those weird socks like a boss. She says she feels like she’s 50 again. Moral of the story? Don’t wait for a fall to listen. Listen now. Your future self will thank you.
Branden Temew
January 7, 2026 AT 17:01So let me get this straight… the solution to a side effect caused by medication… is more medication? And we’re calling this progress? What if the real problem is that we’re medicating aging itself? Maybe the real question isn’t which pill is safest… but why we’re even trying to engineer our way out of natural decline. Just saying.
Frank SSS
January 9, 2026 AT 14:12Yeah yeah yeah. ARBs good. Alpha blockers bad. But who’s gonna pay for the new script? Who’s gonna drive to the pharmacy? Who’s gonna remember to take it? My grandma’s on 14 meds already. She forgets half of them. The system doesn’t care if she stands up dizzy. It just wants the next prescription filled. This post is nice. But it’s not fixing anything.
Paul Huppert
January 9, 2026 AT 23:20My dad’s on lisinopril and he swears by the water trick. 16 oz before getting up. He says it’s like giving his body a head start. Also wears compression socks like it’s fashion. I didn’t believe him until I saw him go from needing a cane to walking the dog without stopping. Small changes. Big difference.