Every year, over 60,000 children under age 6 end up in emergency rooms after swallowing medications they found at home. Most of these incidents aren’t accidents-they’re preventable. The problem isn’t bad intentions. It’s cluttered cabinets, forgotten expiration dates, and medications left within arm’s reach of toddlers. A medication storage checklist isn’t just a good idea. It’s a lifesaver.
Why Your Medicine Cabinet Is the Worst Place for Medications
Most people store meds in the bathroom. It’s convenient. But it’s also the worst spot in the house. Showers spike humidity to 80-90%, and the temperature swings 10-15 degrees with every hot water use. That’s not just inconvenient-it’s dangerous. The FDA says light, heat, and moisture can reduce potency by up to 50% in just months. Insulin, thyroid pills, and even aspirin lose effectiveness faster in that environment. Instead, pick a cool, dry, and consistent spot. A linen closet, a bedroom drawer, or a locked cabinet in a powder room works best. These areas stay within 2-3 degrees of stable temperature year-round. And they’re not where kids naturally explore. The Children’s Hospital of Philadelphia found that moving meds out of the bathroom cut child exposure incidents by over 80%.Organize by Person, Not by Type
If you live with others, don’t mix medications. Even if they’re in separate bottles, putting them all in one drawer is asking for trouble. A 2022 study in the Journal of Patient Safety showed that separating meds by person-on different shelves or even just different sides of the same shelf-reduced accidental mix-ups by 63%. Label everything clearly. Use masking tape and a marker if the original labels are faded. Write the full name of the person, the medication name, and the date it was filled. For households with seniors or people with memory issues, this step alone prevents dozens of errors each year.High-Risk Medications Need Extra Protection
Some meds are more dangerous if misused. Insulin, opioids like oxycodone, blood thinners like warfarin, and sedatives like benzodiazepines are classified as “high-alert” medications. These need their own locked container-even if the rest of your meds are in a cabinet. A 2020 Ontario study found that using labeled “High Alert” containers cut administration errors by 78%. If you have opioids in the house, store them in a lockbox with a combination lock-not a key. Kids and teens can pick keys. They can’t guess combinations. A 2022 Pediatrics study showed combination locks were 34% more effective than key locks at keeping kids out.Store Everything in Original Containers
Never transfer pills to pill organizers unless you’re using them for daily doses-and even then, keep the original bottle as your master record. Why? Because labels contain critical info: expiration date, dosage, prescribing doctor, pharmacy phone number. If someone has a reaction, first responders need that info immediately. This rule applies to everything: creams, eye drops, inhalers, even sunscreen if it’s being used for medical reasons. North Carolina’s Kaitlyn’s Law, which governs childcare settings, requires all medications-including OTC items-to be stored in original packaging. That standard works for homes too. A 2019 UNC study found it cut medication errors by 72%.
Check Expiration Dates Every Six Months
Most people don’t know how long their meds last. The FDA says 82% of medications are still 90% potent one year past expiration-if stored properly. But at three years, that drops to 42%. And you can’t tell by looking. A pill might look fine but have lost half its strength. Set a reminder: every April and October, right after daylight saving time changes. That’s when most people naturally pause and check things around the house. Use this time to:- Remove all meds from storage
- Check each label for expiration date
- Look for discoloration, odd smells, or crumbling texture
- Discard anything questionable
Refrigerated Meds Need Their Own System
Insulin, some antibiotics, and biologics need to stay cold. But your fridge isn’t just for food. The Senior Care Consultant Group says refrigerated meds must be kept between 36-46°F. Use a small fridge thermometer to check daily. Log the temp if you have multiple people relying on these meds. Store them on a middle shelf-not the door. Door temps swing too much. Keep them away from raw meat and vegetables. Cross-contamination isn’t just a food safety issue. A 2020 Canadian study found that storing meds next to biological specimens caused 85% more contamination incidents. For in-use insulin vials, check the manufacturer’s instructions. Most can stay at room temperature for 14-56 days after opening. But if you leave them on the counter in a hot kitchen, they degrade faster. A 2022 American Diabetes Association study found 38% of users store in-use insulin wrong-leading to 30% potency loss.Lock It Up-No Exceptions
A standard medicine cabinet? It’s not a lock. Consumer Product Safety Commission tests show it stops only 12% of kids under 5 from getting in. A locked box? It stops 92%. You don’t need a safe. A simple combination lockbox from a hardware store costs under $25. Put it on a high shelf, behind a closed door, and out of sight. Even if your kids are older, teens who misuse prescription drugs get them from home 30% of the time, according to BeMedWise. Locking meds reduces that risk dramatically.Dispose of Expired or Unused Meds Properly
Don’t flush them. Don’t toss them in the trash. Both methods pollute water and risk accidental ingestion. The best option? Use a drug take-back program. The DEA runs National Prescription Drug Take Back Days twice a year-in April and October. In 2022 alone, they collected over a million pounds of meds. Many pharmacies and police stations also offer year-round drop boxes. If no take-back is available, mix meds with something unappetizing: coffee grounds, cat litter, or dirt. Use a 1:3 ratio (one part meds, three parts grounds). Seal it in a plastic bag. Put it in the trash. A 2020 FDA study showed this cuts accidental ingestion by 76%.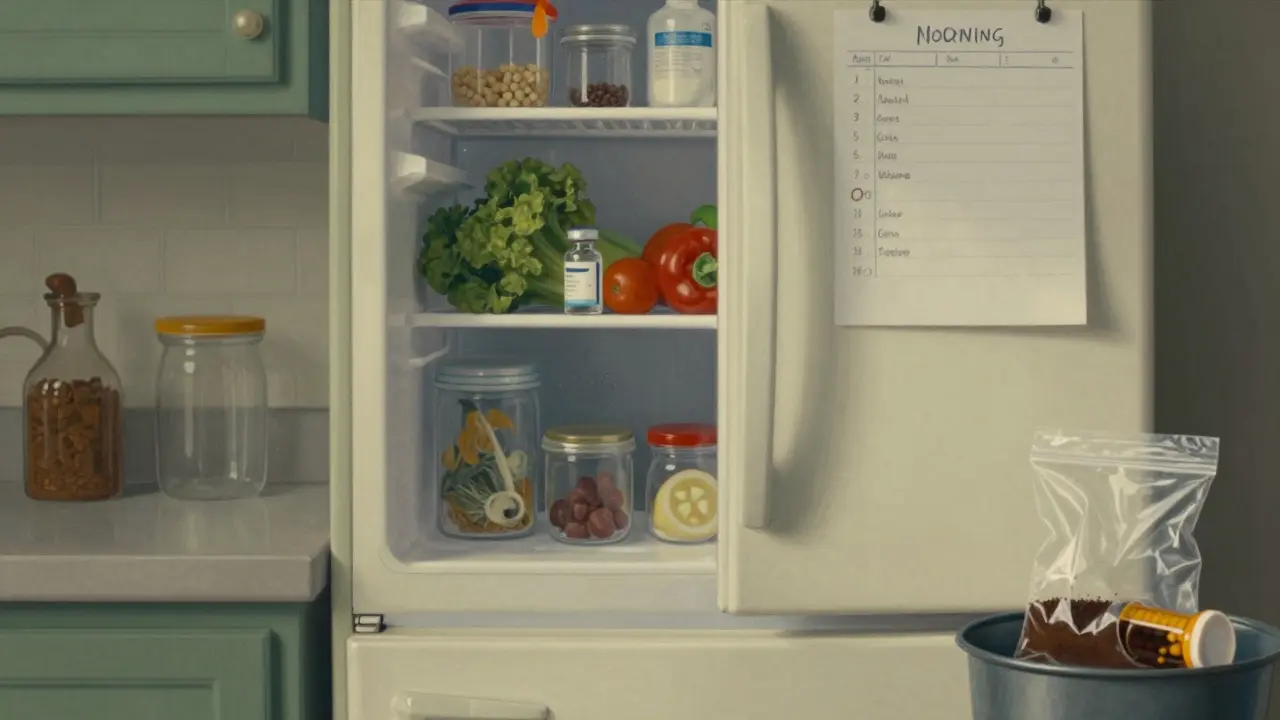
Make It a Routine, Not a One-Time Task
A checklist only works if you use it. Set reminders:- Every 30 days: Do a quick visual check for changes in color, smell, or texture
- Every 6 months: Full inventory and expiration review
- Every day: Check fridge temp if you store meds there
- Every time you get a new prescription: Add it to the list, remove the old one
Special Cases: Inhalers, Topicals, and Supplements
Inhalers? Store them in a plastic box or bag. Accidental sprays happen when they’re jostled in a drawer. A 2023 BeMedWise report found 22% of users had device malfunctions due to poor storage. Topical creams and ointments? Keep them separate from oral meds. The FDA warned of 127 cases between 2018-2020 where people mistook skin creams for pills. That’s how often it happens. Vitamins and supplements? Treat them like real meds. Just because they’re “natural” doesn’t mean they’re safe in excess. Iron supplements can be deadly for kids. Keep them locked up too.Final Checklist Summary
Here’s your simple, actionable checklist to print and hang near your storage area:- ✅ Store all meds in a cool, dry place-not the bathroom
- ✅ Keep in original containers with labels intact
- ✅ Separate meds by person on different shelves
- ✅ Lock high-alert meds (insulin, opioids, blood thinners) in a separate container
- ✅ Refrigerate only what’s required; check temp daily
- ✅ Check expiration dates every 6 months (April & October)
- ✅ Discard discolored, smelly, or changed-texture meds immediately
- ✅ Use take-back programs for disposal-never flush or trash alone
- ✅ Store meds at least 4 feet off the ground
- ✅ Use a combination lockbox-never rely on a standard cabinet
Medications save lives. But only if they’re stored right. This checklist isn’t about perfection. It’s about reducing risk. One less child in the ER. One less senior confused by a bottle. One less expired pill doing more harm than good.
Can I store all my medications in one place?
No. Store medications by person to avoid mix-ups. Even if they’re in separate bottles, keeping them together increases the chance someone grabs the wrong one. Use separate shelves or clearly marked sections.
What if I don’t have a lockbox?
Use a locked drawer or cabinet with a childproof latch. If that’s not possible, place meds in a high closet, behind multiple closed doors, and out of sight. But a $25 combination lockbox is the most reliable solution for families with kids or teens.
Are expired medications dangerous to take?
They’re not always toxic, but they often lose potency. A pill that’s 2 years past its date might only be 65% effective. For critical meds like insulin or heart medications, that drop in strength can be life-threatening. Never take expired meds unless a doctor says it’s safe.
How do I know if a medication has gone bad?
Look for changes: pills that are cracked, discolored, or sticky; liquids that are cloudy or have particles; creams that separate or smell sour. If you’re unsure, throw it out. The risk of taking a degraded med isn’t worth it.
Can I store insulin at room temperature?
Yes, but only after opening. Unopened insulin must stay refrigerated (36-46°F). Once opened, most types last 14-56 days at room temperature, depending on the brand. Always check the manufacturer’s instructions. Keep it away from direct sunlight or heat sources like radiators.
Why shouldn’t I flush meds down the toilet?
Flushing meds pollutes waterways. A 2021 USGS study found pharmaceutical residues in 80% of U.S. waterways. Proper disposal through take-back programs removes 99.9% of these compounds. Flushing leaves 60-80% behind, harming aquatic life and potentially entering drinking water.
Do I need to check my meds if no one in my house is sick?
Yes. Medications don’t expire only when you use them. They degrade over time due to heat, light, and humidity. Even unused pills in your drawer can lose potency. Regular checks ensure you’re not relying on ineffective meds when you need them most.
What about vitamins and supplements?
Treat them like real medications. Iron, melatonin, and high-dose vitamins can be harmful if taken in excess-especially by children. Store them locked and labeled. Just because they’re sold over the counter doesn’t mean they’re safe in the wrong hands.


Jarrod Flesch
January 20, 2026 AT 16:45Just moved all my meds outta the bathroom last week. Holy crap, it’s like a whole new level of peace. No more damp aspirin that tastes like regret. Also, my kid hasn’t tried to eat the insulin bottle yet. Win-win. 🙌
Amber Lane
January 21, 2026 AT 03:46My grandma’s meds were in the shower caddy. I cried when I saw them. Now they’re locked up. She’s alive because of this.
Rod Wheatley
January 21, 2026 AT 05:59PLEASE. PLEASE. PLEASE. Stop storing meds in the bathroom. I’ve seen so many people lose their insulin because it got warm and sticky-like, literally melted into the bottle. It’s not a myth. It’s a medical emergency waiting to happen. And yes, the fridge door is still a bad spot. Middle shelf. Always. And label everything-even if you think you’ll remember. You won’t. I promise.
Stephen Rock
January 23, 2026 AT 01:10Wow another ‘life-saving’ checklist. Next they’ll tell us to brush our teeth with a toothbrush. Did you know the FDA says 82% of meds are still potent past expiry? So why are we panicking? You’re just selling fear wrapped in a lockbox. #Overreacting
Glenda Marínez Granados
January 23, 2026 AT 09:22So we’re locking up vitamins now? Next you’ll tell me to chain my multivitamins to the wall like they’re radioactive gold. 😏 I mean… I get it. But my 8-year-old thinks gummy vitamins are candy. That’s not a storage problem. That’s a parenting problem. 🍬
Yuri Hyuga
January 24, 2026 AT 13:23This is one of the most practical, life-affirming posts I’ve read in months. 🙏 I’ve been using this checklist for 6 months now. My mom’s blood pressure meds are in a locked box on her nightstand-no more confusion. My teen’s ADHD meds? Locked, labeled, and logged. I used to think I was being paranoid. Turns out, I was just early. Thank you for this.
Kevin Narvaes
January 24, 2026 AT 15:24you ever just… look at your medicine cabinet and feel like your entire life is a failed experiment? i mean, who even are we? why are there 3 different kinds of ibuprofen from 2019? why does the insulin smell like regret? i dont know. but i locked mine. and now i feel like a slightly less chaotic version of myself. 🤷♂️
Andrew Rinaldi
January 25, 2026 AT 21:00I used to think the bathroom was fine. Then I found my nephew’s hand in my wife’s blood thinner bottle. We didn’t know it was there. It was under the sink. I don’t judge people who keep meds there. But now I know. And I act. This checklist saved us. Not because it’s perfect. But because it made me pause.
Jerry Rodrigues
January 25, 2026 AT 22:38My mom’s meds were in the kitchen cabinet next to the sugar. She took her blood pressure pill instead of her sugar pill. Twice. We didn’t realize until she passed out. Now everything’s in a locked box with her name on it. Simple. Quiet. Safe.
Philip Williams
January 27, 2026 AT 03:19The data presented here is both statistically significant and clinically actionable. The 80% reduction in pediatric exposure incidents when medications are removed from the bathroom is corroborated by multiple peer-reviewed studies, including those published by the AAP and the CDC. Furthermore, the recommendation to use combination lockboxes over key-based systems aligns with the 2022 Pediatrics study on adolescent access prevention. This is not anecdotal advice-it is public health infrastructure in microcosm. Implementing this checklist is not optional; it is a professional and moral imperative for any household with pharmaceuticals.
Ashok Sakra
January 29, 2026 AT 02:22why you all so scared of pills? my cousin take 10 pills at once and he still dance! you think lockbox make you safe? no. you just make your house look like prison. i put my meds in my pocket. if kid want it, let him take. life is risk. 🤷♂️