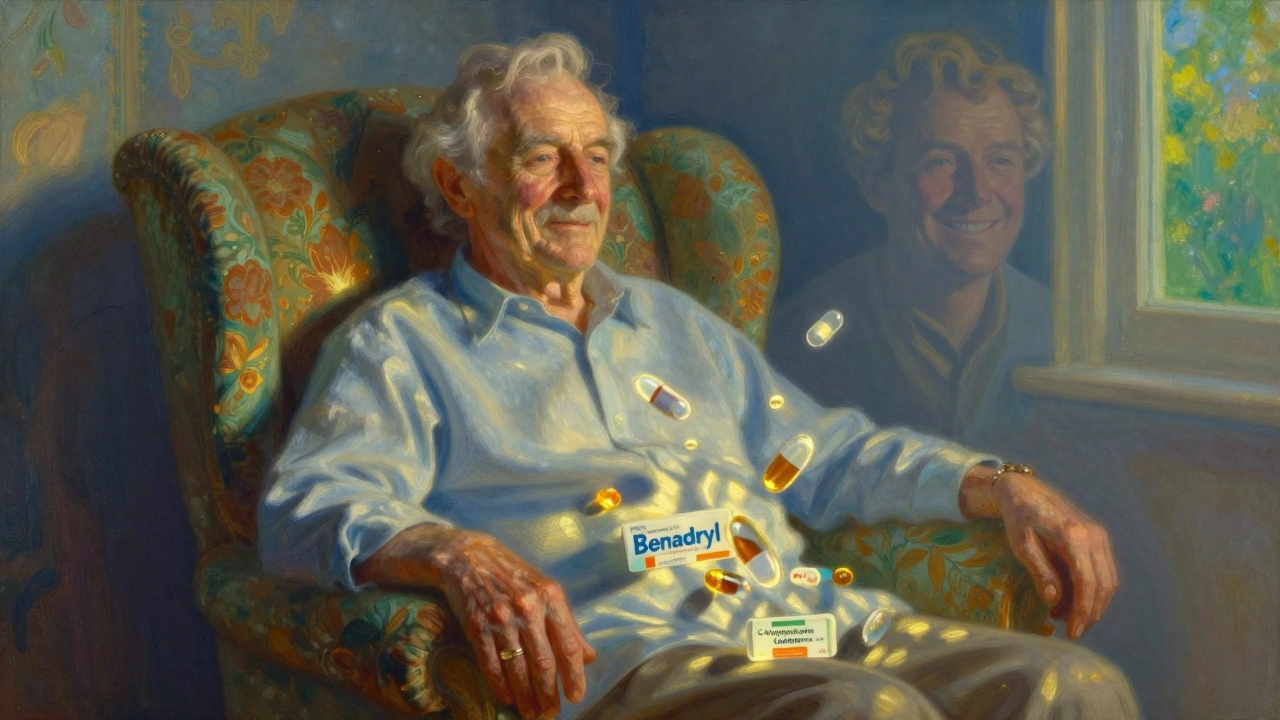
Many older adults are told their memory lapses, confusion, or sluggishness are just part of getting older. But what if those symptoms aren’t aging at all? What if they’re caused by a pill they’re taking every day? This is more common than you think. In fact, up to 70% of seniors take at least one medication that can mimic dementia - and doctors often miss it.
What You’re Seeing Might Be a Drug Reaction
When a senior starts forgetting names, gets lost in familiar places, or seems unusually drowsy or confused, the default assumption is often dementia or Alzheimer’s. But in many cases, the real culprit is a medication. These aren’t rare side effects. They’re widespread, predictable, and often reversible.Anticholinergic drugs are the biggest offenders. These include common over-the-counter sleep aids like Benadryl, bladder control pills like oxybutynin, certain antidepressants, and even some allergy meds. They work by blocking acetylcholine, a brain chemical critical for memory and focus. In younger people, the body handles this fine. In seniors, the brain gets flooded with these drugs because the liver and kidneys can’t clear them as efficiently. Studies show older adults absorb 30-50% more of these drugs into their brains than younger people do.
The symptoms? They look exactly like dementia:
- Sudden confusion or disorientation
- Forgetting recent conversations or appointments
- Feeling like you’re moving in slow motion
- Drowsiness so severe it affects daily tasks
- Blurred vision or trouble reading
- Dizziness that increases fall risk
- Constipation or trouble urinating
These symptoms don’t creep in slowly like Alzheimer’s. They show up fast - often within days or weeks of starting a new drug or changing a dose. And here’s the kicker: when the drug is stopped, symptoms often improve - sometimes dramatically.
Common Medications That Trick the Brain
Not all drugs are created equal. Some are far more likely to cause brain fog in seniors. The American Geriatrics Society’s Beers Criteria - updated in 2019 - lists 30 medications that should generally be avoided in people over 65 because of their cognitive risks.Here are the top culprits:
- Diphenhydramine (Benadryl) - Used for allergies, sleep, or colds. Causes drowsiness in 81% of seniors and confusion in 72%.
- Oxybutynin (Ditropan) - For overactive bladder. Linked to memory loss and delirium.
- Tricyclic antidepressants (e.g., amitriptyline) - Older depression meds. High anticholinergic burden.
- Chlorpheniramine - Found in many cold and allergy combos. Often hidden in multi-symptom formulas.
- Lorazepam (Ativan), alprazolam (Xanax) - Benzodiazepines for anxiety or sleep. Cause short-term memory loss in 65% of seniors.
- Antipsychotics (e.g., quetiapine/Seroquel) - Sometimes prescribed off-label for sleep or agitation. Can cause Parkinson’s-like tremors and worsen confusion.
- Strong opioids (e.g., oxycodone) - Even short-term use leads to memory issues in 57% of older adults.
- Corticosteroids (e.g., prednisone) - Can trigger mood swings, paranoia, or hallucinations.
Many of these are still prescribed routinely. A 2023 study found that nearly half of seniors on multiple medications are taking at least one high-risk drug. And because these drugs are often taken for years, the damage builds up. People taking strong anticholinergics daily for three years have a 49% higher risk of being diagnosed with dementia - even if the dementia was never real to begin with.
How to Tell the Difference Between Aging and Drug Side Effects
It’s not easy. But there are clear clues.Onset matters. Normal aging happens slowly. Medication side effects? They show up fast. If your parent started forgetting things two weeks after beginning a new pill - that’s a red flag.
Fluctuation matters. Seniors on problematic meds often have good days and bad days. One morning they’re sharp, the next they’re lost. True neurodegenerative diseases don’t bounce back like that.
Physical symptoms matter. Dry mouth, constipation, blurry vision, or trouble urinating alongside confusion? That’s the classic combo of anticholinergic overload. These aren’t just side effects - they’re warning signs.
Timing matters. Did symptoms start after a hospital stay, a new prescription, or a dose increase? That’s your biggest clue.
And here’s something most families don’t realize: you don’t need a brain scan to spot this. You need a list - a full, current list of every pill, supplement, and OTC med your loved one takes. Include creams, patches, and herbal products. Many seniors don’t tell doctors about Benadryl because they think it’s harmless. It’s not.

The Anticholinergic Cognitive Burden (ACB) Scale
Doctors now have a tool to measure how much a medication cocktail is affecting the brain. It’s called the Anticholinergic Cognitive Burden (ACB) scale.Each drug is scored:
- 1 = Mild anticholinergic effect
- 2 = Moderate
- 3 = Strong
Add up the scores of all the medications a senior takes. If the total is 3 or higher, they’re at significantly increased risk for cognitive decline. A score of 3+ over three years equals a 49% higher dementia risk.
For example:
- Benadryl (3)
- Oxybutynin (2)
- Amitriptyline (3)
- Lorazepam (1)
Total = 9. That’s a very high risk. Even one strong drug - like Benadryl - can push someone into danger.
Ask your pharmacist to calculate the ACB score for your loved one’s meds. Many pharmacies now offer this as part of a medication review.
What You Can Do Right Now
You don’t have to wait for a doctor’s appointment. Start today.- Make a complete list. Write down every medication, including vitamins, supplements, and OTC drugs. Don’t leave anything out.
- Check the Beers Criteria. Search “2019 Beers Criteria list” online. See if any meds on the list are being taken.
- Calculate the ACB score. Use free online tools or ask a pharmacist. If it’s 3 or above, take action.
- Don’t quit cold turkey. Stopping some meds suddenly can be dangerous. Work with a doctor to taper safely over weeks or months.
- Track changes. Keep a journal: “On Day 7 of stopping Benadryl, Dad remembered his granddaughter’s name.” Small wins matter.
Studies show that 30-40% of seniors labeled with dementia improve significantly after deprescribing high-risk meds. Some even return to their baseline cognitive function.

Why This Is Still Overlooked
Despite the evidence, this problem persists. Why?First, doctors are busy. A 15-minute visit doesn’t leave room to dig through a list of 12 medications.
Second, many providers still believe cognitive decline is inevitable with age. They don’t look for reversible causes.
Third, patients don’t speak up. Seniors often assume their foggy thinking is normal. They don’t connect it to their meds.
And fourth - and this is critical - many of these drugs are sold over the counter. People think, “It’s just Benadryl.” But in seniors, “just Benadryl” can be a silent brain killer.
The Bigger Picture: Medicare and the Future
Good news: things are changing. As of 2023, Medicare’s Annual Wellness Visit requires a medication review. That’s 32.5 million seniors covered. But only 38% of primary care doctors actually do full reviews.Technology is helping. New AI tools are being tested to scan electronic health records and flag high-risk combinations before they’re prescribed. Early versions are 85% accurate.
And research is moving fast. Scientists at Indiana University are developing a simple blood test to measure acetylcholine levels - a direct way to spot anticholinergic overload. It’s not mainstream yet, but it’s coming.
The FDA now requires stronger warnings on 17 high-risk drug classes. And in the EU, new rules have cut inappropriate prescribing by 28%.
This isn’t just about pills. It’s about dignity. It’s about giving seniors back their memory, their independence, their ability to recognize their own grandkids.
Final Thought: Ask the Right Question
Next time you notice a loved one seeming “off,” don’t ask, “Is this dementia?”Ask this instead: “What new meds did they start in the last month?”
That question - simple, direct, and urgent - can change everything. Because sometimes, what looks like aging is just a pill that shouldn’t be there.

Shayne Smith
December 6, 2025 AT 11:03I knew my grandma wasn't just 'getting forgetful'-she started zoning out after they gave her that sleep aid. Took three months and a pharmacist's intervention to realize it was Benadryl. She’s back to telling stories about her childhood like it’s yesterday. Just say no to OTC 'harmless' meds for seniors.
Max Manoles
December 8, 2025 AT 09:42The anticholinergic burden scale is underutilized by primary care physicians, despite robust clinical validation in multiple cohort studies. The Beers Criteria, while widely cited, remains inconsistently implemented due to cognitive load and time constraints in ambulatory settings. A structured medication reconciliation protocol, ideally integrated into EHRs with automated ACB scoring, could reduce iatrogenic cognitive decline by over 40% in patients over 65. Pharmacists must be formally integrated into geriatric care teams.
Rashmi Gupta
December 8, 2025 AT 10:08So now we’re blaming pills for aging? Next you’ll say gravity is a pharmaceutical side effect. People have been forgetting things since before Benadryl was invented. Maybe the real problem is that we’re living longer than our brains evolved to handle.
Kumar Shubhranshu
December 9, 2025 AT 21:40Karen Mitchell
December 10, 2025 AT 17:45This article is dangerously irresponsible. It implies that cognitive decline is always reversible, which is not only medically inaccurate but also encourages patients to discontinue prescribed medications without professional oversight. Such advice could lead to severe withdrawal syndromes, uncontrolled hypertension, or psychiatric decompensation. Responsibility matters.
olive ashley
December 11, 2025 AT 08:22They don’t want you to know this because Big Pharma makes billions off dementia meds. Benadryl? It’s in 70% of OTC sleep aids. The FDA knew. Doctors knew. But why fix a problem when you can sell a pill for it? I’ve seen 3 relatives ‘dementia’-ed by their own medicine cabinet. The system is rigged.
Ibrahim Yakubu
December 13, 2025 AT 00:19In Nigeria, we don’t have this luxury. Our elders take whatever is cheap and available. Sometimes it’s leftover antibiotics or herbal concoctions from the market. No ACB scale, no Beers Criteria-just survival. But I’ve seen the same symptoms: confusion after taking cough syrup with diphenhydramine. This isn’t just an American problem. It’s a global silent epidemic.
Gwyneth Agnes
December 14, 2025 AT 12:11Mansi Bansal
December 16, 2025 AT 12:05It is a matter of profound societal neglect that we have allowed pharmacological iatrogenesis to become normalized in geriatric care. The conflation of age-related physiological decline with drug-induced cognitive impairment constitutes a systemic failure of medical ethics. One must interrogate not merely the pharmacokinetics, but the epistemological bias that renders senescence synonymous with cognitive diminution.
Kay Jolie
December 17, 2025 AT 18:19As a geriatric pharmacist, I’ve seen this play out in real time. The ACB score isn’t just a tool-it’s a lifeline. I had a patient on a cocktail totaling 11: Benadryl, amitriptyline, oxybutynin, lorazepam, and prednisone. She was labeled ‘mild Alzheimer’s.’ After deprescribing, she started knitting again. Her granddaughter cried. That’s not a side effect. That’s a resurrection. We need mandatory ACB reviews for every senior on 3+ meds. Period.