When treating overactive bladder (OAB), Oxytrol is a transdermal patch that delivers oxybutynin continuously for up to 72 hours. While the patch is praised for steady drug levels and fewer oral side effects, many patients wonder how it stacks up against pills, other anticholinergics, and the newer beta‑3 agonist class. This guide breaks down efficacy, side‑effect profiles, cost, and practical considerations so you can see which option fits your lifestyle.
How Oxytrol Works
Oxytrol contains oxybutynin an anticholinergic that relaxes the detrusor muscle. By blocking muscarinic receptors, it reduces involuntary bladder contractions that cause urgency and leakage. The patch bypasses the gastrointestinal tract, delivering a steady 3.9 mg of oxybutynin over three days. This steady‑state avoids the peak‑and‑trough swings seen with oral dosing, which is why many users report less dry mouth and constipation.
Key Differences vs Oral Oxybutynin
Oral oxybutynin is the original tablet form, typically 5 mg two to three times daily. The main contrast points are:
- Absorption: Oral pills undergo first‑pass metabolism, creating an active metabolite (N‑desethyloxybutynin) that contributes to anticholinergic side effects. The patch delivers the parent drug directly into systemic circulation.
- Side‑effect profile: Studies show the patch reduces dry mouth incidence from ~30% (oral) to ~12% (patch) while keeping efficacy comparable.
- Convenience: One patch lasts three days; tablets require daily dosing and may be missed.
- Cost: In the U.S., a 30‑day supply of Oxytrol averages $150-$180, whereas generic oral oxybutynin can be as low as $15-$30.
Comparing Oxytrol to Other Anticholinergics
Several newer anticholinergics aim to improve tolerability. Below are the most common alternatives.
- Solifenacin a selective M3‑receptor blocker taken once daily. It has a lower incidence of dry mouth (≈15%) but can cause constipation.
- Darifenacin another M3‑selective agent, dosed once daily. Efficacy is similar to oxybutynin, yet the side‑effect burden is modestly lower.
- Trospium a quaternary ammonium compound that does not cross the blood‑brain barrier. This reduces cognitive side effects, a concern for older adults.
- Fesoterodine a prodrug of 5‑hydroxy‑oxybutynin, offering flexible dosing (4 mg or 8 mg). It can be titrated to balance efficacy and tolerability.
- Tolterodine the first‑generation anticholinergic, taken twice daily. It’s often a starting point but has a higher dry‑mouth rate than newer agents.
When you line these up against the Oxytrol patch, three themes emerge: steady plasma levels, reduced gastrointestinal side effects, and higher cost. The oral agents may be cheaper, but patients who struggle with dry mouth or who need once‑daily dosing often prefer the newer pills.
Beta‑3 Agonist Alternative: Mirabegron
Mirabegron a beta‑3 adrenergic receptor agonist that relaxes the bladder detrusor muscle via a different pathway offers a non‑anticholinergic option. Key points:
- Mechanism: Works on adrenergic receptors, so it avoids classic anticholinergic side effects like dry mouth and constipation.
- Efficacy: Clinical trials show mirabegron’s reduction in incontinence episodes is comparable to oral oxybutynin.
- Side‑effects: Can raise blood pressure and cause headaches; otherwise well‑tolerated.
- Cost: Branded mirabegron (Myrbetriq) costs about $200-$250 for a 30‑day supply, though a generic version (now available) brings the price down to $120‑$150.
For patients with a history of anticholinergic intolerance, mirabegron is often the first alternative. Some clinicians even combine a low dose of mirabegron with an anticholinergic for synergistic effect, but that strategy should be guided by a urologist.
Side‑Effect Summary
Side‑effects can be the deal‑breaker. Below is a quick snapshot:
- Dry mouth: Oxytrol ≈ 12%, oral oxybutynin ≈ 30%, solifenacin ≈ 15%, mirabegron ≈ 2%.
- Constipation: Higher with anticholinergics (up to 20%); mirabegron ≈ 5%.
- Cognitive impact: Notable with high‑dose oral anticholinergics, minimal with trospium and mirabegron.
- Blood pressure: Mirabegron may raise systolic BP by 3‑5 mmHg; other agents have neutral effect.
Cost & Insurance Considerations
Insurance coverage varies widely. Generic oral anticholinergics (e.g., oxybutynin, tolterodine) are almost always covered with low co‑pays. Oxytrol, being a brand‑name patch, often lands in a higher tier, leading to co‑pays of $30‑$50. Newer agents like solifenacin and mirabegron have generic forms that are slowly gaining formulary acceptance, but many plans still label them “specialty.” When budgeting, factor in:
- Monthly out‑of‑pocket cost.
- Potential need for dose adjustments (some drugs have multiple strengths).
- Whether a pharmacy‑discount program or manufacturer coupon is available.
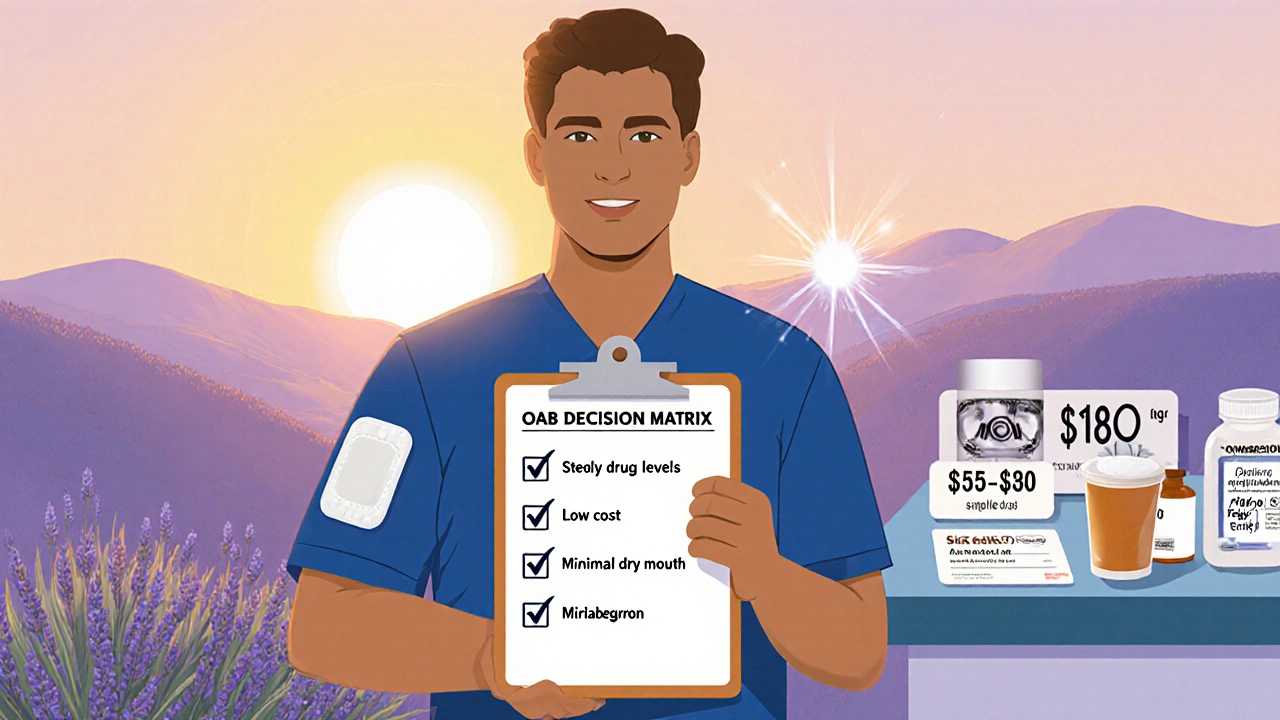
Choosing the Right Option: Decision Checklist
Use this quick checklist to match your priorities with the best medication.
| Priority | Best Fit | Why |
|---|---|---|
| Steady drug levels, minimal dosing hassle | Oxytrol | 3‑day patch, fewer peaks/troughs |
| Low cost, generic availability | Oral oxybutynin or tolterodine | Generics under $30/month |
| Reduced dry mouth & constipation | Solifenacin or mirabegron | Selective or non‑anticholinergic mechanism |
| Avoid cognitive side effects (elderly) | Trospium or mirabegron | Doesn’t cross blood‑brain barrier |
| Combine for maximal efficacy | Low‑dose mirabegron + low‑dose anticholinergic | Synergistic effect, lower individual dosing |
Talk with your provider about these factors. A short trial of two weeks on a patch can reveal tolerability, while oral agents often need a titration period.
Full Comparison Table
| Medication | Formulation | Typical Dose | Key Efficacy (UUI ↓ %) | Common Side‑Effects | Average US Cost* | Best For |
|---|---|---|---|---|---|---|
| Oxytrol | Transdermal patch | One 3.9 mg patch q72 h | ≈ 45 % reduction | Dry mouth (12 %), skin irritation | $150‑$180 | Patients who struggle with oral meds |
| Oral oxybutynin | Tablet | 5 mg 2-3×/day | ≈ 45 % reduction | Dry mouth (30 %), constipation | $15‑$30 | Cost‑sensitive users |
| Solifenacin | Tablet | 5 mg once daily | ≈ 40 % reduction | Dry mouth (15 %), constipation | $90‑$120 | Those preferring once‑daily dosing |
| Trospium | Tablet | 20 mg twice daily | ≈ 38 % reduction | Constipation (12 %), blurred vision | $80‑$110 | Elderly patients, cognitive risk |
| Mirabegron | Tablet | 25 mg once daily (max 50 mg) | ≈ 42 % reduction | Elevated BP, headache | $120‑$250 | Patients intolerant to anticholinergics |
*Costs are average retail prices in the United States (2025) and can vary by pharmacy, insurance, and coupons.
Practical Tips for Starting a New OAB Medication
- Start low, go slow - many drugs have a titration schedule to reduce side‑effects.
- Keep a bladder diary for at least one week before and after switching.
- Check blood pressure after the first week on mirabegron.
- Rotate patch sites (upper arm, abdomen, back) to avoid skin irritation.
- Ask your pharmacist about discount cards; they can shave $30‑$50 off a month’s supply.
When to Call Your Doctor
If you notice any of the following, reach out promptly:
- Severe dry mouth that interferes with swallowing.
- Sudden increase in heart rate or blood pressure > 140/90 mmHg.
- Persistent skin rash or blister at the patch site.
- Worsening urinary symptoms after 2-3 weeks of therapy.
Early communication helps adjust the regimen before complications become entrenched.
Bottom Line
Oxytrol offers a convenient, steady‑release option that cuts the classic anticholinergic side‑effects for many users, but it carries a higher price tag. Oral anticholinergics remain budget‑friendly, while newer agents like solifenacin and mirabegron give targeted benefits for specific tolerability concerns. Use the decision matrix and comparison table to match your priority-cost, dosing simplicity, or side‑effect profile-to the right medication.
Can I switch from Oxytrol to an oral anticholinergic without a washout period?
Yes. Because both contain oxybutynin, a brief overlap isn’t harmful, but you should remove the patch before starting the first tablet to avoid excess dosing.
Is the Oxytrol patch safe for people with heart disease?
Generally yes, but anticholinergics can increase heart rate slightly. Discuss any arrhythmia history with your cardiologist before starting.
How long does it take for Oxytrol to start working?
Therapeutic levels are reached within 24‑48 hours, but most patients notice a reduction in urgency after about a week of consistent use.
Can I use Oxytrol if I’m pregnant?
Oxybutynin is classified as FDA Pregnancy Category C. It should only be used if the benefit outweighs potential risk, and always under close medical supervision.
What should I do if the patch falls off prematurely?
Replace it immediately with a fresh patch at a clean, dry site. If you’re within 24 hours of the next scheduled change, you can keep the extra patch for backup.


Vijaypal Yadav
October 20, 2025 AT 20:05From a pharmacokinetic standpoint, the Oxytrol patch sidesteps the hepatic first‑pass effect that plagues oral oxybutynin. By delivering the parent compound directly into systemic circulation, it yields a more stable plasma concentration curve. This steadiness translates into fewer peaks that would otherwise trigger anticholinergic side‑effects. The metabolite N‑desethyloxybutynin, responsible for much of the dry‑mouth burden, is markedly reduced with transdermal delivery. Clinical trials have shown a roughly 60 % drop in reported xerostomia compared with the tablet form. Moreover, the 72‑hour dosing interval eliminates the daily pill fatigue that many patients describe. The patch’s adhesive technology also allows for site rotation, mitigating localized skin irritation. Overall, the pharmacological rationale behind Oxytrol is sound, especially for patients who are sensitive to gastrointestinal side‑effects.
Kate McKay
October 27, 2025 AT 17:45That explanation really nails the why behind the patch. It helps to see the science broken down into everyday terms.
Matthew Hall
November 3, 2025 AT 16:25Honestly, the patch feels like the drama queen of OAB meds.
Ron Lanham
November 10, 2025 AT 15:05When we consider the broader implications of prescribing a high‑cost, brand‑only solution such as Oxytrol, we must first acknowledge the ethical responsibility of the clinician to balance efficacy with accessibility. It is not merely a question of pharmacodynamics; it is a question of social justice, of ensuring that the patient who cannot afford a $180 monthly supply is not left to suffer in silence. The patch’s convenience, while genuine, may inadvertently create a two‑tiered system wherein only those with robust insurance coverage reap its benefits. One could argue that this perpetuates a form of medical elitism, reinforcing disparities that have long plagued our healthcare system. Furthermore, the incremental reduction in dry mouth, though statistically significant, does not fully mitigate the lingering anticholinergic burden that many elderly patients experience, especially when cognitive side‑effects are considered. The patch’s skin irritation potential, often downplayed in promotional literature, can become a source of chronic discomfort, leading to non‑adherence. In the grand scheme, the modest efficacy advantage does not unequivocally outweigh the economic and psychosocial costs imposed on a vulnerable population. Therefore, the prescribing physician must exercise prudence, perhaps reserving Oxytrol for a subset of patients who have demonstrably failed cheaper alternatives. Ultimately, the decision should arise from a shared decision‑making process that transparently addresses both clinical outcomes and financial implications, lest we sacrifice patient autonomy at the altar of pharmaceutical convenience.
Andrew Hernandez
November 17, 2025 AT 13:45Oxytrol literally drops the pill in your skin and lets you forget about it. Cheap alternatives exist but the patch is neat.
laura wood
November 24, 2025 AT 12:25I totally get why someone would love the patch for its hassle‑free schedule. It’s also nice to hear that the side‑effects are milder for many folks.
Israel Emory
December 1, 2025 AT 11:05Indeed, the patch’s simplicity is appealing, however, one must also weigh the financial strain, especially given that insurance tiers often categorize it as a specialty product, leading to higher co‑pays; additionally, the potential for skin irritation, albeit low, should not be dismissed, as it can affect adherence; finally, consider that not all patients respond equally, so a trial period with close monitoring is advisable.
Sebastian Green
December 8, 2025 AT 09:45Thanks for laying that out. I’ll keep an eye on how my skin reacts if I try it.
Alex Pegg
December 15, 2025 AT 08:25While many tout the patch’s convenience, the data still shows comparable efficacy across all anticholinergics, so the premium price is hard to justify without a clear superiority claim.
Wesley Humble
December 22, 2025 AT 07:05In a rigorously controlled environment, the reduction in xerostomia from approximately 30 % to 12 % constitutes a statistically significant improvement (p < 0.01). Moreover, the pharmacodynamic profile of transdermal oxybutynin demonstrates a lower peak‑to‑trough fluctuation ratio, which plausibly underlies the observed tolerability benefits. Nonetheless, the cost–benefit analysis must incorporate the incremental $130‑$150 out‑of‑pocket expense, which may be prohibitive for many patients. 🧐
Mahesh Upadhyay
December 29, 2025 AT 05:45Numbers aside, isn’t it just another way for pharma to charge more for the same effect?
Rajesh Myadam
January 5, 2026 AT 04:25Both perspectives have merit; the clinical benefits are real, yet the financial barrier is a legitimate concern that clinicians should discuss openly with patients.
Kirsten Youtsey
January 12, 2026 AT 03:05One cannot help but notice the subtle undercurrent of pharmaceutical lobbying that shapes these comparative narratives, steering both prescribers and patients toward brand‑locked solutions while the generic counterparts languish in obscurity, a phenomenon that deserves vigilant scrutiny.