Doctor Appointment Preparation Tool
Preparation Checklist
Your preparation score: 25% - Keep adding information to improve.
Medication List Builder
Your Medication List
Symptom Tracker
Your Symptom List
Discussion Points & Questions
Key Discussion Points
Suggested Questions to Ask
What to Bring Checklist
Essential Documents
Health Information
Preparation Tips
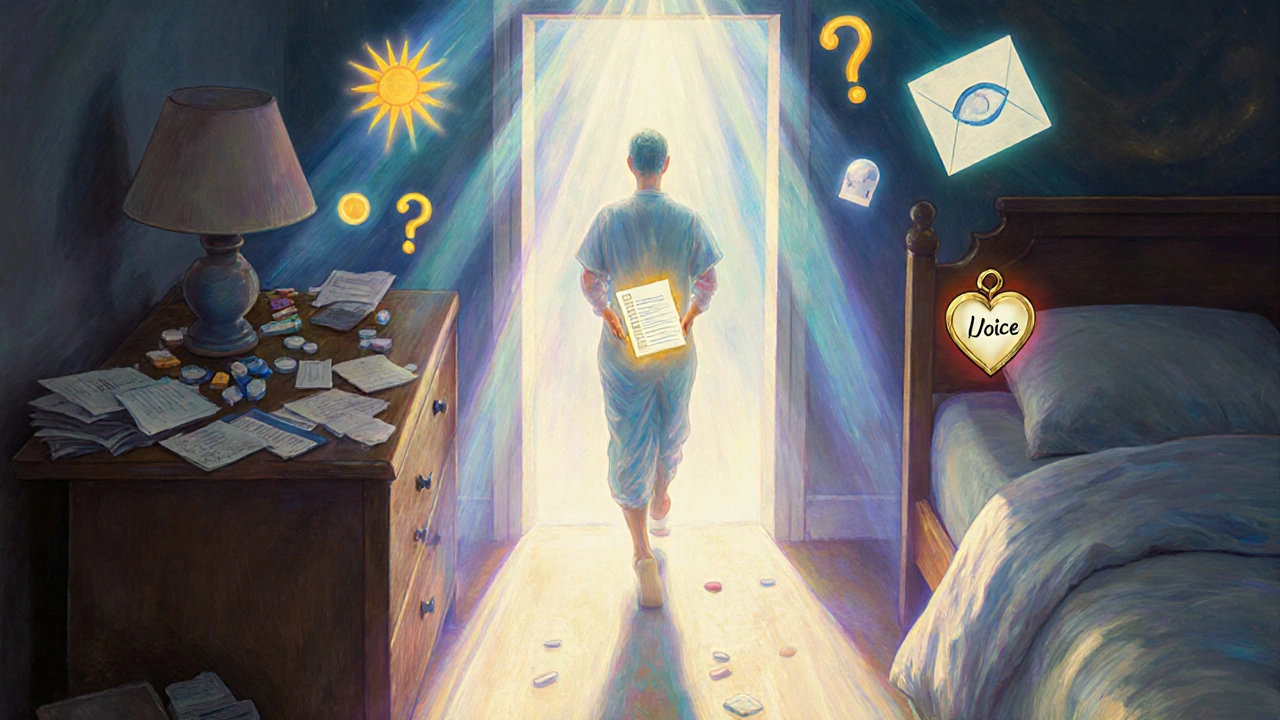
What to Bring to Your Doctor Appointment
Walking into a doctor’s office without being prepared is like showing up to a job interview with no resume. You might still get through, but you’re leaving a lot on the table. The truth is, most patients don’t bring the right things-and it costs them. Mayo Clinic data shows that patients who arrive with a complete medication list have 37% fewer medication errors during their visit. That’s not a small gap. That’s life-changing.
Start with the basics. Bring your health insurance card and a government-issued photo ID. Sounds obvious, but clinics in Sydney and across Australia report that nearly 1 in 5 patients forget one or the other. Then, bring any forms your doctor’s office asked you to fill out ahead of time. If you didn’t get any, ask when you book the appointment. Many clinics now send digital forms via email or patient portals.
Now, the big one: your medication list. Don’t just say, “I take blood pressure pills.” Write it down. Include every pill, patch, liquid, or supplement-even the ones you only take when you feel bad. For each one, list:
- Drug name (e.g., Lisinopril)
- Strength (e.g., 10mg)
- Dosage (e.g., one tablet)
- When you take it (e.g., every morning with breakfast)
- Why you take it (e.g., for high blood pressure)
- Who prescribed it (e.g., Dr. Patel, Sydney Heart Clinic)
- When you started (e.g., January 2023)
Don’t rely on memory. Use your pharmacy app, a pill organizer label, or even a photo of your medicine cabinet. If you’re unsure about a supplement, bring the bottle. Many patients forget that things like fish oil, vitamin D, or herbal teas can interact with prescriptions. Aurora Health Care’s checklist includes this exact detail-and their data shows 45% of initial medication lists are incomplete or wrong. Don’t be part of that statistic.
Bring your family health history if you have it. Not just “my dad had a heart attack.” Be specific: “My father had a heart attack at age 56. My mother has type 2 diabetes since 2015. My paternal grandmother died of ovarian cancer at 68.” This helps your doctor spot patterns you might not even know matter.
And don’t forget your wearable data. If you use a Fitbit, Apple Watch, or Garmin, bring your recent activity and sleep logs. AdventHealth’s 2023 update now pulls wearable data directly into patient prep tools. Even if your doctor doesn’t ask, having this info ready can turn a vague “I feel tired” into “I’ve averaged 5.2 hours of sleep for 3 weeks straight.” That’s powerful.
What to Talk About During Your Appointment
Your time with the doctor is short. Make it count. Don’t wait until the end to say, “Oh, and I’ve been having headaches.” Lead with what matters most.
Start with your symptoms. But don’t say, “I’ve been feeling off.” Use numbers and timing. For example:
- “I’ve had sharp pain in my lower back for 3 weeks, mostly after sitting at my desk.”
- “I get dizzy 2-3 times a week, usually when I stand up too fast.”
- “My anxiety spikes every night around 10pm-I’ve been waking up drenched in sweat.”
Include intensity. Rate it on a scale of 1 to 10. Say, “It’s a 7 when I walk, but a 3 when I’m resting.” This tells your doctor how it’s affecting your life.
Don’t skip lifestyle details. Doctors need to know how you live-not just how you feel. Be honest about:
- Alcohol: “I have 2 glasses of wine on weekends.”
- Exercise: “I walk 20 minutes, 4 days a week.”
- Smoking: “I quit cigarettes in 2022, but I vape 5 pods a week.”
- Sleep: “I’m up at least twice a night. Can’t fall back asleep.”
- Stress: “My job’s been overwhelming since my mom passed.”
AdventHealth’s guidelines stress this: doctors can’t help with lifestyle-related issues if you don’t tell them. And they’re trained not to judge. Hiding facts won’t protect you-it just delays care.
Bring up anything you’ve been putting off. That weird rash. The mood swings. The trouble remembering names. The fact that you haven’t had a bowel movement in 4 days. None of it’s too small. Cleveland Clinic’s research shows patients who list 3-5 key concerns have an 89% chance of getting them resolved. Those who don’t prepare? Only 63%.

Questions to Ask Your Doctor
Don’t just nod and say “yes” to everything. Ask questions. The right ones can change your treatment path.
Here are seven proven questions from Mayo Clinic’s communication protocol:
- Why are you recommending this test or treatment?
- What are the possible side effects or risks?
- Are there simpler, safer, or cheaper options?
- What happens if I don’t do anything?
- What would you recommend if I were your parent or child?
- How will I know if this is working?
- When should I come back or call if things get worse?
These aren’t just polite questions-they’re tools. When patients ask “What would you recommend if I were your mother?” they get more honest answers. Studies show doctors are more likely to share uncertainty or alternative options when framed this way.
Also ask about next steps. Don’t leave without knowing:
- When you’ll get test results
- Who to contact if symptoms change
- Whether you need a follow-up appointment
- If you need referrals (to a specialist, physio, dietitian)
Write these down. Or better yet, record the appointment on your phone (ask permission first). You’ll forget half of what’s said once you’re out the door.
How to Use Technology to Prepare
Most clinics now use digital tools to make appointments smoother. If yours doesn’t, ask why.
Cleveland Clinic’s AppointmentPass® system lets you check in online, upload documents, and even answer symptom questions before you arrive. Patients using it save 22 minutes on average and have 19% more complete records. If your doctor uses MyChart, Apple Health, or Google Fit, connect them. Mayo Clinic’s app (version 4.7.2) can pull your pharmacy records from 27 major chains and sync with your fitness tracker automatically.
Ambetter Health now updates your medication list automatically when you refill a prescription. That means no more guessing what you took last week. AdventHealth’s AI tool, LiveWell, scans your past visits and suggests questions you might have forgotten. It’s not magic-it’s data.
If you’re not tech-savvy, don’t worry. You don’t need an app. Just write things down. Use your phone’s Notes app. Or grab a notebook. The goal isn’t to use fancy tech-it’s to be ready.
Common Mistakes and How to Avoid Them
Here’s what most people get wrong-and how to fix it.
- Mistake: Bringing a vague list like “I take pills for my heart.” Fix: Write exact names, doses, and times. Use your pharmacy label.
- Mistake: Waiting until the last minute to think about what to say. Fix: Spend 10 minutes the night before writing down your top 3 concerns.
- Mistake: Not asking questions because you’re nervous. Fix: Write your questions on a sticky note. Read them aloud before you go.
- Mistake: Assuming your doctor knows your full history. Fix: Even if you’ve been seeing them for years, update them. Things change.
- Mistake: Forgetting to bring your glasses, hearing aid, or cane. Fix: Pack them like you would your wallet or phone.
St. Joseph Hospital Bangor’s study found that patients who prepared a written list of concerns had 26% higher satisfaction scores. They felt heard. They got answers. They left confident.
What to Do After Your Appointment
The appointment isn’t over when you walk out. That’s when the real work begins.
Right after you leave, jot down what was said. What did the doctor recommend? What tests were ordered? What’s the next step? If you didn’t write it down during the visit, do it now. Memory fades fast.
If you were given a prescription, confirm the pharmacy details. Is it in-network? Do you need prior authorization? Ambetter Health’s mail-order system can deliver meds to your door-but only if you set it up before you leave.
Set a reminder to follow up. If your doctor said, “Call in two weeks if it hasn’t improved,” put that in your calendar. Don’t wait for them to call you.
And if something feels off after the visit-like a new symptom, a confusing instruction, or a side effect you didn’t expect-call the office. Don’t wait. Most clinics have a nurse line or patient portal for quick questions.
Preparing for your doctor’s visit isn’t about being perfect. It’s about being present. It’s about making sure your voice is heard. And when you do it right, you don’t just get better care-you get better outcomes. Less guesswork. Fewer repeat visits. More clarity. That’s worth the 20 minutes you spend before you walk in the door.
What if I forget to bring my medication list?
If you forget your list, don’t panic. Tell your doctor what you remember: the names of your main prescriptions, what they’re for, and how often you take them. Many clinics now have access to your pharmacy records through secure systems like MyChart or the National Electronic Health Transition Authority (NEHTA) in Australia. Still, bringing your own list is faster and more accurate. It’s the best way to avoid errors.
Should I bring a family member to my appointment?
Yes, especially if you’re dealing with a new or complex condition. A second set of ears helps you remember what was said. They can also ask questions you might forget. Make sure the clinic knows they’re coming-some places need written permission to share your health info with others. Bring them as your support, not your decision-maker. You’re still in charge.
How far in advance should I prepare for my appointment?
Start 24-48 hours before. Spend 15 minutes gathering your meds, writing down symptoms, and thinking of questions. Don’t wait until the morning of. Stress makes it harder to think clearly. If you’re using a digital tool like MyChart or Apple Health, start syncing data a week ahead. The earlier you prepare, the less you’ll forget.
What if I’m too nervous to speak up?
Write your concerns down ahead of time-even if you think they’re silly. Bring the paper with you. Read it aloud if you need to. Most doctors expect patients to be nervous. They’ve heard it all. Being quiet won’t protect you-it just delays answers. You’re not being difficult. You’re being smart.
Do I need to bring my medical records from other doctors?
Not usually. Most Australian clinics can request records electronically through the My Health Record system. But if you’ve seen a specialist recently or had tests done outside your usual network, bring a copy of the summary report. It saves time and avoids duplicate tests. If you’re unsure, call the clinic ahead of time and ask.


Corra Hathaway
November 21, 2025 AT 13:29Clifford Temple
November 22, 2025 AT 00:47Simone Wood
November 22, 2025 AT 09:36Sheldon Bazinga
November 23, 2025 AT 20:28Paula Jane Butterfield
November 25, 2025 AT 19:31Kartik Singhal
November 26, 2025 AT 21:47Chris Vere
November 27, 2025 AT 13:33Pravin Manani
November 27, 2025 AT 23:51Mark Kahn
November 28, 2025 AT 23:02Leo Tamisch
November 30, 2025 AT 06:47Daisy L
December 1, 2025 AT 14:57Sandi Moon
December 2, 2025 AT 17:32