When your doctor suspects a blockage in your urinary tract or wonders if your kidneys are shrinking, they often reach for one tool first: renal ultrasound. It’s quick, safe, and doesn’t zap you with radiation like a CT scan. For patients with flank pain, a history of kidney stones, or high blood pressure, this simple scan can answer critical questions-Is there a blockage? How big are the kidneys? Is the blood flow still normal? The answers help decide whether you need surgery, medication, or just more monitoring.
What Renal Ultrasound Actually Shows
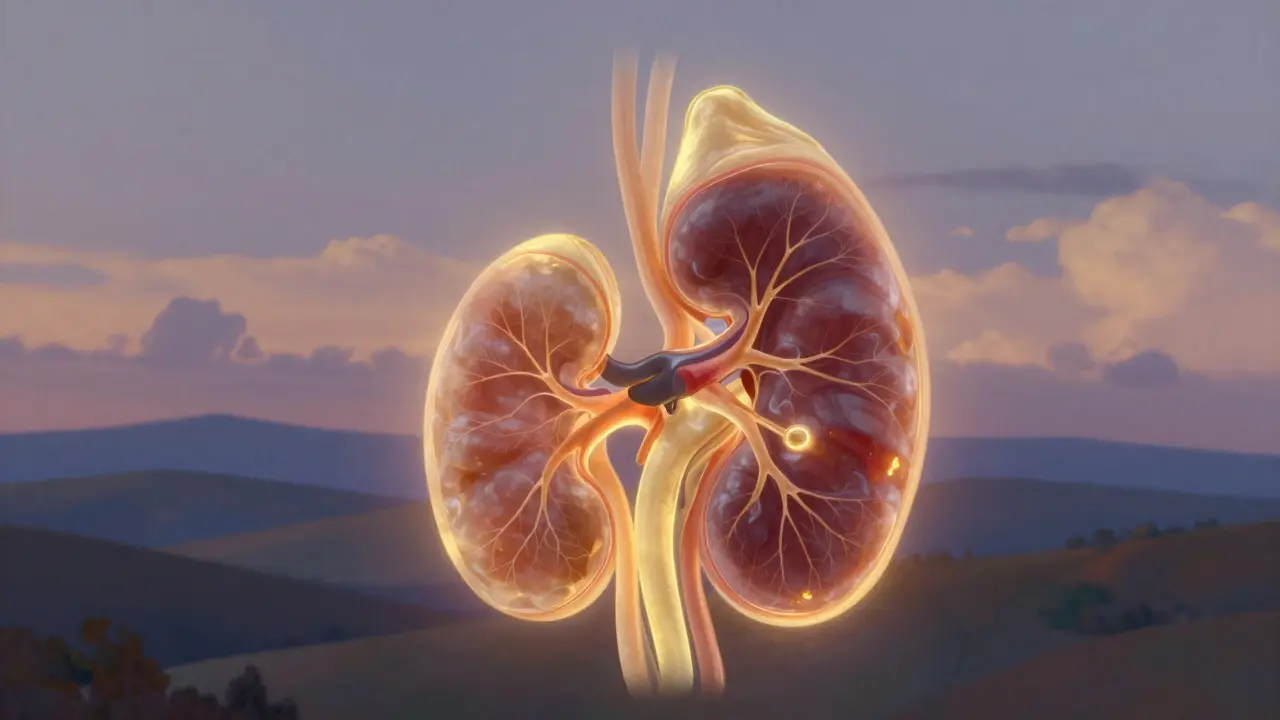
Renal ultrasound uses sound waves, not X-rays, to create real-time images of your kidneys and bladder. It measures three key things: size, shape, and signs of blockage. Normal adult kidneys are about 9 to 13 centimeters long-roughly the size of a fist. If one kidney is significantly smaller, it might mean long-term damage from high blood pressure, chronic infection, or past obstruction. Cortical thickness-the outer layer of kidney tissue-should be over 1 centimeter. Thinning here signals scarring or loss of functional tissue.
The most common sign of obstruction is hydronephrosis. That’s when urine backs up into the kidney because it can’t drain properly. Think of it like a clogged sink: the basin fills up, and pressure builds. On ultrasound, this shows up as dark, fluid-filled spaces inside the kidney called the renal pelvis and calyces. A normal pelvis diameter is under 7 millimeters. Above that, it’s considered dilated-and the higher the number, the worse the backup.
How Obstruction Changes Blood Flow
Ultrasound doesn’t just take pictures-it also listens. Using Doppler technology, it measures how fast blood flows through the tiny arteries inside the kidney. One number matters most: the resistive index (RI). It’s calculated from the speed of blood flow during heartbeats. A healthy kidney has an RI below 0.70. Once it climbs above that, it’s a red flag.
A 2015 study in the Nigerian Journal of Clinical Practice found that an RI of 0.70 or higher correctly identified obstructive uropathy in 87% of cases, with 90% accuracy. That’s better than many blood tests. Why? When urine backs up, pressure builds in the kidney. That pressure squeezes the tiny blood vessels, making it harder for blood to flow. The heart has to pump harder, and the waveform changes. The RI captures that change. It’s not perfect-obesity, diabetes, or advanced kidney disease can also raise RI-but in the right context, it’s a powerful clue.
Comparing Ultrasound to Other Imaging
CT scans are often seen as the gold standard. They find tiny stones, show exact anatomy, and even track how fast urine drains. But they expose you to radiation-about 10 millisieverts per scan. That’s like 3 years of natural background radiation. For someone with recurrent kidney stones, repeated CTs add up fast.
MRI and nuclear scans have their uses too. MR urography gives detailed images without radiation, but it costs 3 to 5 times more than ultrasound and still misses small stones. Nuclear scans measure kidney function, but they involve radioactive tracers and don’t show structure well.
Ultrasound wins in three areas: safety, speed, and cost. A typical renal ultrasound costs $200-$500 in the U.S., takes 15-30 minutes, and requires no prep. You can do it in the ER, the clinic, or even at the bedside. Emergency doctors use point-of-care ultrasound to rule out obstruction in minutes, cutting diagnosis time by nearly an hour compared to waiting for formal imaging.

When Ultrasound Falls Short
It’s not magic. Ultrasound struggles in people with high body weight. Sound waves can’t penetrate thick layers of fat well. When BMI exceeds 35, the image quality drops sharply. One nephrologist at Mayo Clinic noted that in obese patients, ultrasound often becomes unreliable-and they’re forced to use CT or MRI instead.
It also can’t tell you exactly how fast urine is draining. A CT scan with a special 3D algorithm can measure drainage rate. Ultrasound can’t. It shows dilation, but not the flow. That’s why some patients still need a follow-up scan or nuclear test if the diagnosis is unclear.
And then there’s the operator. A 2018 study found that inexperienced sonographers could measure kidney length with up to 20% variation compared to experts. That’s a big deal when you’re tracking changes over time. Training matters. The American Institute of Ultrasound in Medicine recommends at least 40 supervised exams before someone can reliably interpret renal scans.
Advanced Techniques on the Horizon
Ultrasound is evolving. New tools like shear-wave elastography measure how stiff the kidney tissue is. When urine backs up, pressure builds-and the tissue gets stiffer. Studies from 2013 show this stiffness increases linearly with obstruction. It’s not mainstream yet, but hospitals are testing it for monitoring patients after surgery.
Even more exciting is super-resolution ultrasound. Researchers are now able to see tiny blood vessels inside the kidney that were invisible before. This could let us spot early signs of scarring or reduced blood flow long before kidney function drops. One 2024 review in Nature Reviews Nephrology even suggests this might one day let us count individual nephrons-the filtering units of the kidney-without a biopsy.
Artificial intelligence is also stepping in. Some systems now automatically detect hydronephrosis and grade its severity. That reduces human error and makes monitoring easier for patients who need weekly checks after kidney surgery.
What the Numbers Mean in Practice
Let’s say a 48-year-old man comes in with sudden left-sided pain. His ultrasound shows:
- Left kidney length: 11 cm (normal)
- Right kidney length: 8 cm (small)
- Left renal pelvis diameter: 15 mm (dilated)
- Left RI: 0.78
- Right RI: 0.65
That’s a classic picture. The right kidney is small-likely chronically damaged. The left kidney is swollen and has high resistance. He probably has a stone stuck in the ureter. The RI confirms it’s not just swelling-it’s pressure affecting blood flow. He’ll likely need a stent or lithotripsy.
Now imagine a 72-year-old woman with chronic kidney disease. Her left kidney is 10 cm, right is 9 cm. Pelvis diameter is 6 mm. RI is 0.72 on both sides. No dilation. But the RI is borderline high. That suggests she’s got subtle, long-term pressure on both kidneys-maybe from an enlarged prostate or bladder issues. She doesn’t need surgery, but she needs regular monitoring.
Why It’s Still the First Step
Despite all the fancy tech out there, renal ultrasound remains the starting point for a reason. It’s safe for pregnant women. It’s ideal for kids. It’s affordable. It’s fast. It doesn’t require contrast dye, which can harm kidneys. And it can be repeated as often as needed-weekly, even daily-without risk.
Over 12 million renal ultrasounds are done in the U.S. every year. Nearly every hospital uses it. The American College of Radiology gives it the highest rating (8-9 out of 9) for initial evaluation of suspected obstruction. That’s higher than CT.
It’s not about replacing other tools. It’s about using the right tool at the right time. Ultrasound tells you if there’s a problem. CT tells you what the problem is. Together, they save lives.
What Patients Should Know
You don’t need to fast or prep for a renal ultrasound. Drink water if you’re thirsty-it helps fill the bladder and gives a clearer view. The scan is painless. A gel is applied to your skin, and a probe is moved over your back and sides. You might feel slight pressure, but no pain.
Results are often available right away. In an emergency, the doctor may tell you the findings before you leave. In a clinic, expect a written report within a few days.
Don’t be surprised if your doctor orders more tests later. Ultrasound is a great first step, but not always the last. If the scan is unclear, or if you have symptoms that don’t match the images, further testing is normal.
Can renal ultrasound detect kidney stones?
Yes, but not always. Ultrasound detects about 80% of kidney stones larger than 3 millimeters. Smaller stones, especially those in the ureter, are harder to see. CT scans are better at finding tiny stones, but ultrasound is still preferred for initial screening because it avoids radiation. If ultrasound doesn’t show a stone but symptoms strongly suggest one, a CT may follow.
Is renal ultrasound safe during pregnancy?
Yes, it’s the safest imaging option for pregnant women. Unlike CT or X-rays, ultrasound uses no ionizing radiation. It’s commonly used to evaluate kidney swelling, infection, or obstruction in pregnant patients-especially since urinary tract issues are common during pregnancy due to pressure from the growing uterus.
Why does my doctor check both kidneys?
Comparing both kidneys helps spot problems. A kidney that’s smaller than the other may have chronic damage. A kidney with more dilation than the other likely has a blockage. Even the blood flow (resistive index) should be similar. Differences between sides are often the first clue to disease.
What does a high resistive index mean?
A resistive index (RI) above 0.70 suggests increased resistance to blood flow inside the kidney, often due to pressure from urine backup. It’s a strong indicator of obstruction, especially if it’s only on one side. But it can also rise in chronic kidney disease, diabetes, or advanced age. So it’s not a standalone diagnosis-it’s one piece of the puzzle.
Can ultrasound show kidney scarring?
Indirectly. Ultrasound can’t show scar tissue directly, but it can show its effects: thinning of the kidney’s outer layer (cortex), reduced size, or abnormal texture. If the cortex is less than 1 cm thick, it usually means long-term damage. Newer techniques like elastography are starting to detect stiffness changes linked to scarring, but standard ultrasound still relies on size and shape clues.