What Is Retinal Vein Occlusion?
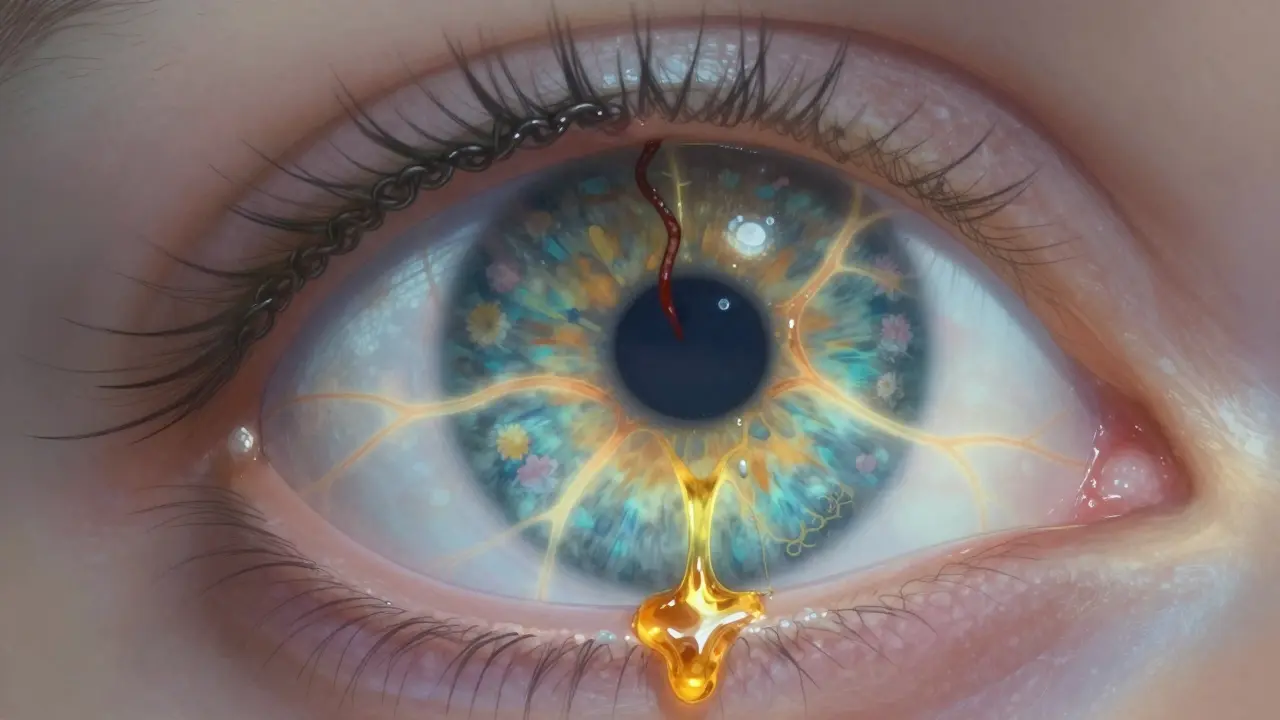
Retinal vein occlusion (RVO) happens when a vein in the retina - the light-sensitive layer at the back of your eye - gets blocked. This blockage stops blood from draining properly, causing fluid to leak into the retina. The result? Swelling, bleeding, and often sudden vision loss in one eye. It’s not painful, but it’s serious. You might notice blurred vision, dark spots, or even complete vision loss in part of your visual field.
There are two main types: central retinal vein occlusion (CRVO), which affects the main vein, and branch retinal vein occlusion (BRVO), which hits smaller branches. BRVO is more common and often happens where a hardened artery presses down on a vein, like a kinked garden hose. CRVO tends to be more severe and affects overall vision more dramatically.
RVO is not rare. Around 16.4 million people worldwide have it, and it’s one of the top causes of vision loss in people over 50. While it can strike younger people, over 90% of CRVO cases happen after age 55. The good news? Treatment has improved dramatically in the last decade - especially when it comes to injections.
Who’s at Risk for Retinal Vein Occlusion?
Most people who get RVO have one or more underlying health problems. The biggest risk factor? High blood pressure. Up to 73% of people over 50 with CRVO have uncontrolled hypertension. Even if you don’t feel symptoms, high blood pressure slowly damages the tiny blood vessels in your eyes. That’s why regular eye checks are so important - especially if you’re over 50 and have high blood pressure.
Diabetes is another major player. About 10% of RVO patients over 50 have diabetes, and those with poor blood sugar control are at higher risk for worse vision outcomes. High cholesterol also plays a role - about 35% of RVO patients have total cholesterol above 6.5 mmol/L. These numbers aren’t just statistics; they’re warning signs your body is under vascular stress.
Glaucoma increases your risk too. When pressure inside your eye is too high, it can squeeze the retinal vein, especially near the optic nerve. If you have glaucoma and notice sudden vision changes, don’t wait - get checked right away.
Lifestyle matters. Smoking doubles your risk. Obesity and lack of movement contribute to poor circulation and thicker blood, both of which make clots more likely. In younger patients - under 45 - the cause is often different. Oral contraceptives are a known trigger, especially for CRVO in women. Blood disorders like polycythemia vera or inherited clotting conditions like factor V Leiden can also be culprits. If you’re under 45 and get RVO, your doctor will likely order blood tests to rule these out.
How Are Injections Used to Treat RVO?
The blockage itself can’t be undone, but the damage it causes - especially fluid buildup in the macula (macular edema) - can be treated. That’s where injections come in.
Anti-VEGF drugs like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) are the first-line treatment. These drugs block a protein called VEGF that causes abnormal blood vessels to grow and leak fluid. By stopping VEGF, they reduce swelling and often improve vision.
Clinical trials show impressive results. In the BRAVO trial, patients on ranibizumab gained an average of 16.6 letters on an eye chart after a year. That’s the difference between barely reading a menu and reading it clearly. Aflibercept did even better in patients with very poor starting vision. In the COPERNICUS trial, patients gained over 18 letters on average.
Bevacizumab, originally developed for cancer, is used off-label because it’s much cheaper - around $50 per dose compared to $2,000 for the branded versions. Many clinics, especially public hospitals, use it widely. Studies show it works just as well for many patients.
For patients who don’t respond well to anti-VEGF drugs, or who can’t handle frequent injections, dexamethasone implants (Ozurdex) are an alternative. This tiny, biodegradable pellet releases steroid slowly over 3-6 months. In the GENEVA study, nearly 28% of CRVO patients gained 15 or more letters of vision with Ozurdex - nearly double the rate of those who got a placebo.

What to Expect During and After an Eye Injection
Getting an injection in your eye sounds scary - and for some, it is. But the procedure is quick and usually painless. Your eye is numbed with drops, cleaned with antiseptic, and held open with a tiny clip. The needle goes in for just a second. Most people feel pressure, not pain.
Afterward, you might see floaters or have a red spot on the white of your eye. That’s normal. About 25-30% of patients get a small bleed under the conjunctiva. Temporary blurriness and mild discomfort are common too. Serious complications like infection (endophthalmitis) are rare - happening in less than 1 in 1,000 injections.
The real challenge isn’t the procedure - it’s the commitment. Most patients need monthly injections for the first 3-6 months. Then, depending on how your eye responds, your doctor will switch to an “as needed” schedule. Real-world data shows people with RVO typically get 8-12 injections in the first year.
That’s a lot of visits. Some patients develop injection anxiety. One patient on a support forum said, “My heart races every time I walk in. I know it’s routine, but I still feel like I’m going to lose my vision.” Others feel overwhelmed by the cost. A single Lucentis injection can cost $150 after insurance - and that’s just one of many.
Why Some People Don’t Respond to Injections
Not everyone improves. About 20-30% of patients don’t respond well to anti-VEGF drugs. Why? It’s not always clear. Sometimes the swelling is too long-standing, and the retina has already started to scar. Other times, the underlying cause - like uncontrolled diabetes or high blood pressure - keeps driving the problem.
Doctors now use OCT scans to track progress. If the central subfield thickness (CST) stays above 300 microns after 3-4 injections, it’s a sign the treatment isn’t working. That’s when they consider switching to a steroid implant or combining treatments.
Some patients do better with steroids from the start. Research shows those with baseline vision worse than 20/200 often respond better to Ozurdex than to anti-VEGF. Others with better starting vision do best with anti-VEGF. There’s no one-size-fits-all. Treatment is becoming more personalized.

The Future of RVO Treatment
The future is moving away from monthly shots. New approaches are being tested to reduce the burden.
The Port Delivery System (Susvimo), originally approved for macular degeneration, is now in trials for RVO. It’s a tiny refillable implant placed in the eye that slowly releases ranibizumab for up to 6 months. If it works, patients could go from monthly visits to twice a year.
Gene therapy is another frontier. RGX-314, currently in Phase II trials, uses a harmless virus to deliver a gene that makes your eye produce its own anti-VEGF protein. Imagine one treatment that lasts years.
There’s also OPT-302, a new drug that blocks a different form of VEGF. Early studies show it works better when combined with aflibercept - especially for stubborn cases.
Doctors are also using advanced imaging like OCT angiography to predict who will respond to what treatment. Instead of guessing, they’ll be able to match the right drug to the right patient based on their eye’s unique biology.
What You Can Do Now
If you’ve been diagnosed with RVO, the most important thing is to stick with your treatment plan. Vision can improve - but only if you keep getting the injections when needed. Missing appointments can mean permanent damage.
Control your risk factors. Get your blood pressure, blood sugar, and cholesterol checked regularly. Quit smoking. Move more. Eat better. These aren’t just general health tips - they’re critical to preventing another blockage in your other eye or worsening the one you already have.
If cost is a barrier, ask your doctor about bevacizumab. It’s safe, effective, and widely used. Many insurance plans cover it. Don’t assume you can’t afford treatment - there are options.
And if you’re struggling with the emotional toll - the anxiety, the fatigue, the fear - talk to someone. Support groups, online forums, even your eye care team can help. You’re not alone.
When to Call Your Doctor
- Sudden vision loss or worsening blurriness
- Pain, redness, or light sensitivity after an injection
- Flashes of light or new floaters
- Difficulty seeing in dim light or recognizing faces
Don’t wait. Even if you think it’s just “another bad day,” it could be a sign your RVO is getting worse or that you’ve developed a new complication like neovascular glaucoma.

Robyn Hays
December 27, 2025 AT 17:59Caitlin Foster
December 28, 2025 AT 14:15Andrew Gurung
December 29, 2025 AT 19:12Will Neitzer
December 30, 2025 AT 10:46Liz Tanner
January 1, 2026 AT 02:34Nikki Thames
January 1, 2026 AT 03:32James Bowers
January 3, 2026 AT 01:34Babe Addict
January 4, 2026 AT 23:38Jane Lucas
January 6, 2026 AT 11:57Elizabeth Alvarez
January 8, 2026 AT 08:45Miriam Piro
January 9, 2026 AT 21:08Paula Alencar
January 11, 2026 AT 04:06