Understanding Supraventricular Tachycardia (SVT) and Its Impact on Driving
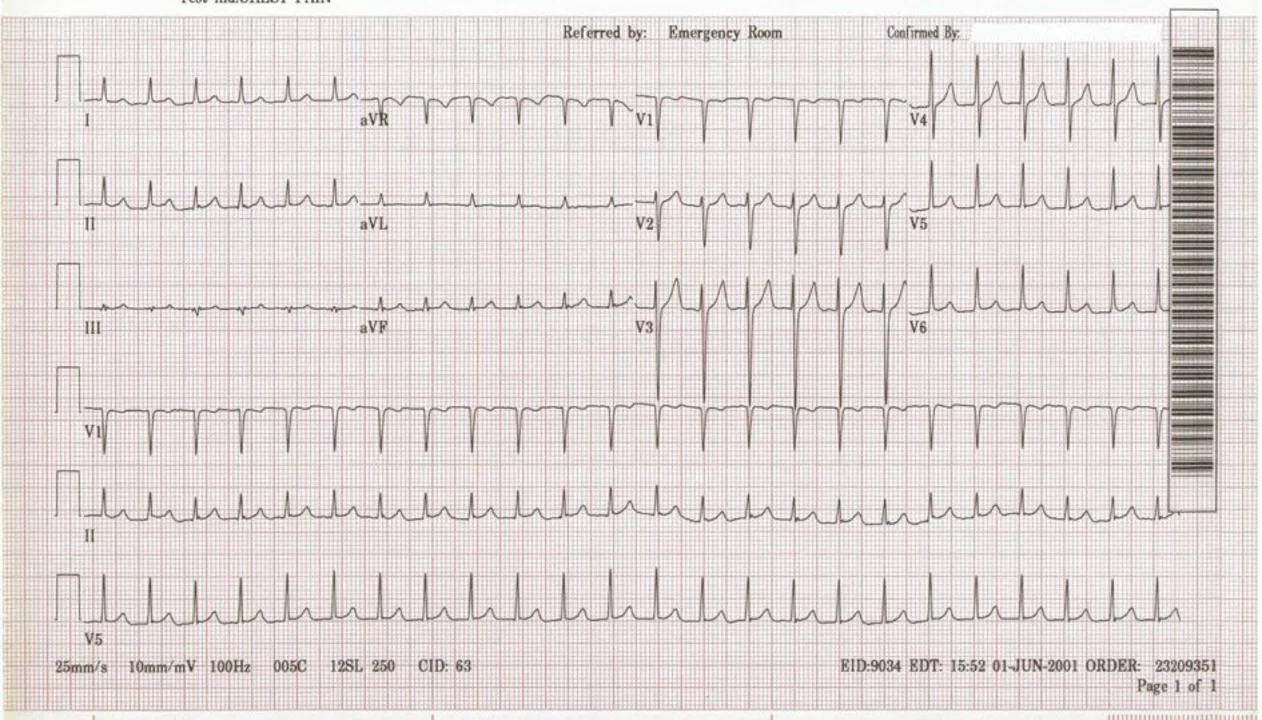
As someone who has experienced supraventricular tachycardia (SVT), I understand how frightening and disorienting it can be. SVT is a type of abnormal heart rhythm that originates in the upper chambers of the heart, causing a rapid heartbeat. This can lead to dizziness, shortness of breath, chest pain, and even fainting. Naturally, these symptoms can have a significant impact on our ability to drive safely.
In this article, I will share some essential safety tips and guidelines for those of us with SVT who want to continue driving. It's crucial to have a clear understanding of our condition and how it affects our everyday lives, including our time behind the wheel. So let's dive in and explore the relationship between SVT and driving.
Discussing Your Condition with Your Healthcare Team
The first and most important step in managing SVT and driving is to have an open dialogue with your healthcare team. Your doctor or cardiologist will be able to provide you with personalized advice based on your specific condition, symptoms, and medical history. They can also recommend any necessary adjustments to your treatment plan to help you stay safe on the road.
Make sure to discuss any concerns you have about your ability to drive safely. Your healthcare provider may recommend certain restrictions, such as avoiding driving during episodes of SVT or limiting your driving to short distances. Always follow their advice to ensure your safety and the safety of others on the road.
Recognizing the Warning Signs of an SVT Episode
One of the keys to managing SVT while driving is being able to recognize the warning signs of an episode. These may include a sudden rapid heartbeat, dizziness, shortness of breath, or chest pain. If you notice any of these symptoms while driving, it's important to pull over as soon as it is safe to do so.
Once you've safely pulled over, take a few moments to focus on your breathing and try to relax. In many cases, SVT episodes can be terminated by performing certain maneuvers, such as the Valsalva maneuver or carotid sinus massage. However, always consult with your healthcare team before attempting these maneuvers to ensure they're appropriate for your specific situation.
Staying Prepared for an SVT Episode While Driving
Since SVT episodes can occur unexpectedly, it's essential to be prepared for the possibility of an episode while driving. Here are a few tips to help you stay prepared:
- Keep a list of your current medications and a brief description of your medical history in your glove compartment or wallet. This information can be invaluable to first responders in the event of an emergency.
- Carry your cell phone with you at all times and make sure it's charged and easily accessible. This will allow you to call for help if you experience an SVT episode while driving.
- Consider informing a family member, friend, or coworker of your condition and let them know what to do in case of an emergency.
- Always wear your seatbelt and ensure your vehicle is well-maintained and in good working order.
Adjusting Your Driving Habits for a Safer Experience
Adapting your driving habits can also help to minimize the risk of an accident due to an SVT episode. Consider the following adjustments to enhance your safety on the road:
- Avoid driving during times when you're more likely to experience an SVT episode, such as during periods of high stress or when you're feeling fatigued.
- Plan your trips in advance, and give yourself plenty of time to reach your destination. This can help to reduce stress and decrease the likelihood of an SVT episode while driving.
- Practice defensive driving techniques, such as maintaining a safe following distance, scanning the road ahead, and being aware of your surroundings. These practices can help you react more quickly and effectively in the event of an SVT episode.
- Consider enrolling in a defensive driving course or refresher course to improve your driving skills and increase your confidence on the road.
Reevaluating Your Ability to Drive Safely
Finally, it's important to regularly reevaluate your ability to drive safely, especially if your condition or symptoms change. Discuss any changes in your symptoms or overall health with your healthcare team, and seek their guidance on whether it's still safe for you to drive.
Remember, the safety of yourself and others on the road should always be the top priority. By staying informed about your condition, following your healthcare team's advice, and making necessary adjustments to your driving habits, you can continue to enjoy the freedom and independence that driving provides while also minimizing the risks associated with supraventricular tachycardia.

Rich Martin
May 14, 2023 AT 23:33People keep whining about SVT like it's some cosmic punishment, but the truth is simple: if you know the triggers, you can outsmart the rhythm. Stop letting fear dictate your schedule; plan, prep, and pull over when the heart spikes. The road belongs to anyone who respects the limits of their own physiology. Don't let a beating heart become a death sentence.
Buddy Sloan
May 15, 2023 AT 00:33Sending you a big hug and hoping every drive feels safe and calm 😊
SHIVA DALAI
May 15, 2023 AT 02:20The interplay between supraventricular tachycardia and vehicular operation demands a meticulous appraisal of both physiological parameters and legal ramifications. In the annals of cardiological literature, SV‑T is frequently portrayed as a transient perturbation, yet its episodic nature can precipitate profound hemodynamic instability. When a driver experiences a sudden acceleration of the cardiac rhythm, the resultant dizziness or presyncope may compromise the essential faculties required for safe navigation. Accordingly, it becomes incumbent upon the afflicted individual to engage in a comprehensive dialogue with the attending physician, elucidating the frequency, duration, and precipitating factors of each episode. The clinician, in turn, must weigh the therapeutic regimen against the intrinsic demands of motor vehicle operation. Moreover, statutory guidelines in numerous jurisdictions prescribe mandatory reporting or temporary driving restrictions for patients with uncontrolled arrhythmias. This bureaucratic overlay, while seemingly onerous, serves the paramount purpose of safeguarding public welfare. Nevertheless, the psychosocial toll of enforced immobility cannot be understated, as autonomy and the sense of self are intimately linked to the ability to traverse one’s environment. To mitigate this, patients are urged to adopt preemptive strategies, such as maintaining an up‑to‑date medication list within arm’s reach and ensuring reliable communication devices are operational. The Valsalva maneuver, carotid sinus massage, and other termination techniques, when performed under medical supervision, may furnish a rapid resolution to an incipient episode. It is vital, however, that these interventions be rehearsed in a safe setting prior to implementation on the roadway. In addition, the incorporation of stress‑reduction modalities-mindfulness meditation, regulated breathing, and adequate sleep hygiene-can attenuate the incidence of arrhythmic triggers. From a logistical standpoint, scheduling travel during periods of reduced physiological stress and avoiding peak traffic congestion constitute prudent measures. The adoption of defensive driving courses further embellishes the driver’s skill set, rendering them better equipped to respond to unforeseen exigencies. Ultimately, the decision to resume or continue driving must be predicated upon a dynamic assessment, revisited whenever clinical status evolves. In closing, the convergence of medical insight, personal vigilance, and adherence to legislative mandates fosters an environment wherein individuals with SVT can safely partake in the liberty that automobile travel affords.
Vikas Kale
May 15, 2023 AT 04:20From a pathophysiological perspective, SVT represents an autonomic dysregulation that can precipitate abrupt hemodynamic compromise during motorized transit. Empirical data suggest that immediate termination maneuvers-namely the Valsalva technique or carotid sinus massage-restore sinus rhythm in upwards of 70% of acute episodes. Thus, integrating these protocols into your driving contingency plan is not merely advisable but operationally essential. Moreover, the pharmacokinetic profile of beta‑blockers or calcium channel blockers should be synchronized with anticipated travel windows to minimize breakthrough tachyarrhythmias. In practice, maintaining a portable medication log and a fully charged cellular device aligns with industry best‑practice guidelines for arrhythmia management on the road :) Finally, periodic reassessment with your electrophysiologist will calibrate risk stratification and ensure compliance with both clinical and DMV regulations.
Deidra Moran
May 15, 2023 AT 06:30One cannot help but notice that the government’s hidden agenda often uses medical conditions like SVT to impose draconian driving bans on unsuspecting citizens. They claim public safety while covertly augmenting surveillance capabilities through mandatory reporting systems. It is wise to scrutinize every recommendation and demand transparent evidence before surrendering your mobility. Remember, independence is the first line of defense against authoritarian overreach.