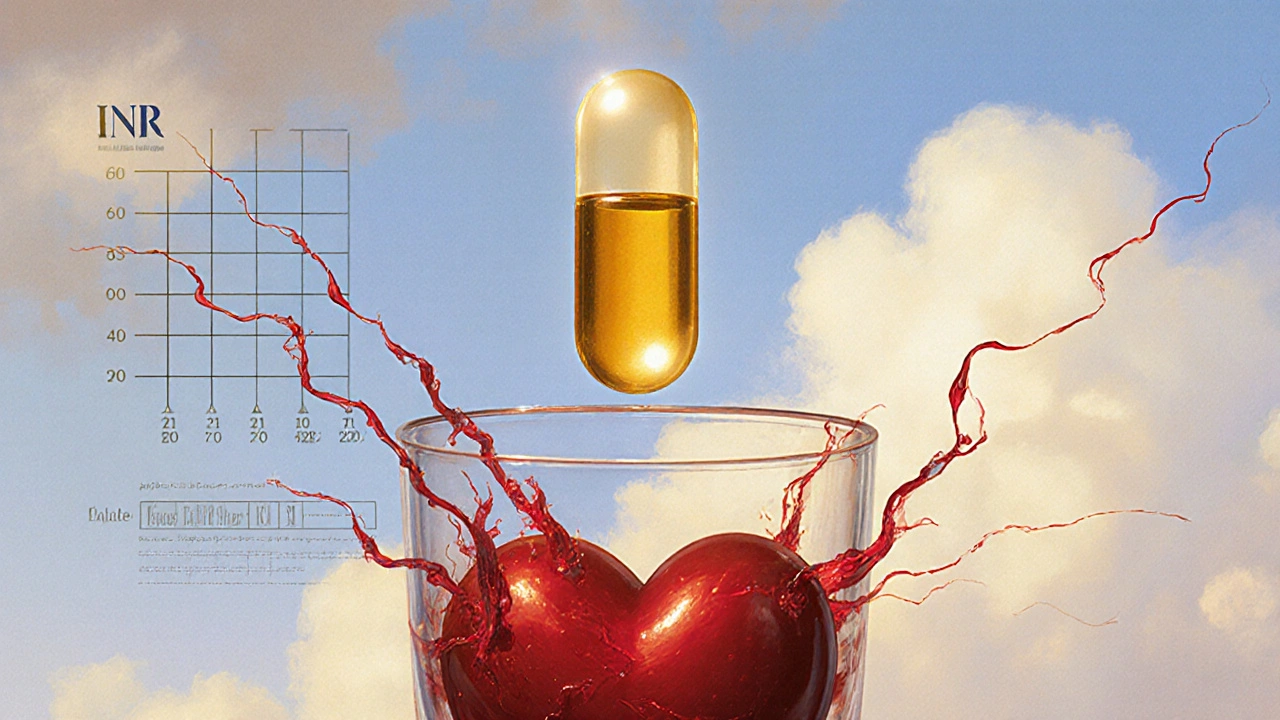
Vitamin E and Warfarin: What You Need to Know About the Interaction
When you take vitamin E, a fat-soluble antioxidant that supports skin health and immune function. Also known as alpha-tocopherol, it's commonly found in nuts, seeds, and supplements. along with warfarin, a blood thinner prescribed to prevent dangerous clots in people with atrial fibrillation, artificial heart valves, or deep vein thrombosis. Also known as Coumadin, it works by blocking vitamin K-dependent clotting factors., you’re mixing two things that both affect how your blood clots. It’s not just a theory—studies and real-world cases show this combo can make your blood too thin, raising your risk of bruising, nosebleeds, or worse.
Here’s the thing: vitamin E doesn’t work the same way as warfarin, but it can still tip the balance. Warfarin slows clotting by targeting vitamin K. Vitamin E, especially in doses over 400 IU daily, may interfere with platelet function and reduce clotting on its own. When you stack them, the effect isn’t just added—it’s multiplied. People on warfarin who start taking high-dose vitamin E supplements often see their INR numbers jump unexpectedly. That’s not a fluke. It’s a known interaction, documented in clinical reports and pharmacy safety databases. And no, you can’t just adjust your warfarin dose on your own. Even if you feel fine, a spike in INR can lead to internal bleeding without warning signs.
It’s not just about supplements. Some multivitamins, fish oil blends, and even certain herbal products contain vitamin E in hidden amounts. If you’re on warfarin, you need to check every label—not just the ones labeled "vitamin E." The same goes for your doctor and pharmacist. Many patients don’t mention supplements unless asked directly. But if you’re taking anything beyond a basic daily vitamin, your provider needs to know. A simple INR check and a quick conversation can prevent a hospital visit.
What about low doses? If you’re getting vitamin E from food—almonds, spinach, sunflower seeds—you’re fine. The risk comes from concentrated supplements. The FDA doesn’t regulate supplement potency the same way it does drugs, so one bottle might have 100 IU and another 800 IU under the same name. That’s why consistency matters. If you’ve been stable on warfarin for months, adding a new supplement—even one labeled "natural"—is a gamble.
You don’t have to quit vitamin E entirely. But you do need to be smart. Talk to your doctor before starting or stopping any supplement. Keep a written list of everything you take—prescriptions, OTC meds, herbs, vitamins—and bring it to every appointment. Watch for signs like unexplained bruising, blood in urine or stool, or unusually heavy periods. These aren’t normal. They’re red flags.
The posts below cover real cases, practical advice, and safety checks from people who’ve walked this path. You’ll find guides on how to track your meds, what to ask your pharmacist, and how to spot hidden interactions in everyday products. Whether you’re on warfarin, thinking about vitamin E, or just trying to stay safe while managing multiple supplements, these resources give you the facts—not the fluff.
Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
Vitamin E supplements can increase bleeding risk when taken with warfarin, especially at doses above 400 IU daily. Learn what the evidence says, which doses are dangerous, and how to stay safe while on anticoagulant therapy.