Weight Loss Surgery: What It Is, Who It Helps, and What You Need to Know
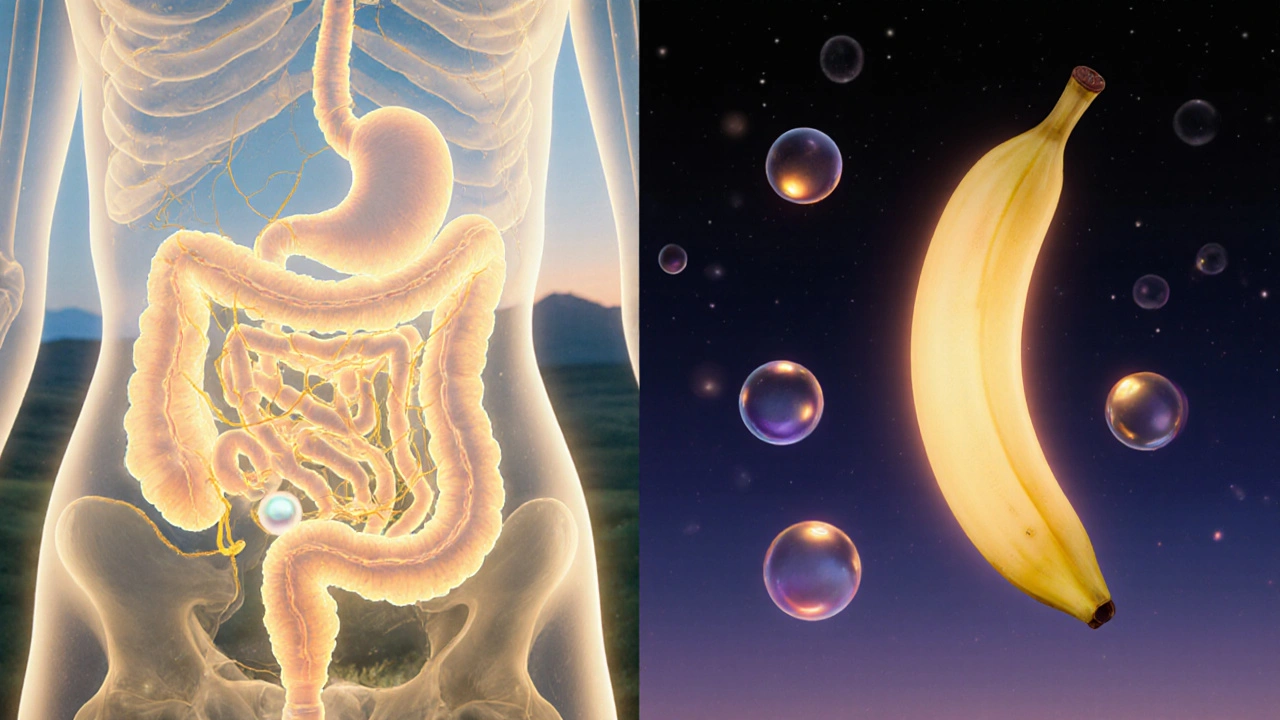
When we talk about weight loss surgery, a group of medical procedures designed to help people with severe obesity lose weight by changing how the stomach and intestines process food. Also known as bariatric surgery, it’s not cosmetic—it’s a treatment for a chronic disease that affects metabolism, heart health, and lifespan. Unlike diets that fail for most people long-term, these surgeries physically limit how much you can eat and sometimes change how your body absorbs calories and signals hunger.
There are several types of weight loss surgery, medical procedures that alter the digestive system to promote significant, sustained weight loss. The most common include gastric bypass, a procedure that creates a small stomach pouch and reroutes the small intestine to reduce calorie absorption, sleeve gastrectomy, where about 80% of the stomach is removed to limit food intake and reduce hunger hormones, and adjustable gastric banding, which uses a band to restrict stomach size. Each has different risks, recovery times, and long-term effects on nutrition and health.
These procedures aren’t for everyone. Doctors typically recommend them when someone has a BMI over 40, or over 35 with serious health problems like type 2 diabetes, high blood pressure, or sleep apnea. Insurance often requires proof that you’ve tried other methods first. But success isn’t just about the surgery—it’s about lifelong changes in eating, movement, and mental health. People who stick with follow-up care, take vitamins, and attend support groups see the best results.
What you won’t find in most ads is how these surgeries affect other parts of your health. Many patients see their diabetes go into remission. Blood pressure drops. Joint pain eases. But side effects like nutrient deficiencies, dumping syndrome, or gallstones are real. That’s why understanding what comes after surgery matters just as much as the procedure itself.
The posts below give you clear, no-fluff facts about how these surgeries work, who they help most, what the real risks are, and how they connect to other health issues—from medication interactions to long-term nutritional needs. You’ll see how weight loss surgery intersects with things like hormone changes, drug safety, and chronic disease management. No marketing. No hype. Just what you need to know if you’re considering this path—or helping someone who is.
Bariatric Surgery: Gastric Bypass vs. Sleeve Gastrectomy - What You Really Need to Know
Gastric bypass and sleeve gastrectomy are the two most common weight loss surgeries. Learn how they differ in weight loss, risks, recovery, and long-term outcomes to make an informed decision.