Amebiasis Treatment
When dealing with Amebiasis Treatment, the medical approach used to eliminate an infection caused by the parasite Entamoeba histolytica. amoebiasis therapy, the goal is simple: kill the parasite, cure symptoms, and prevent relapse. Amebiasis treatment isn’t just a single pill; it combines proper diagnosis, the right drug choice, and follow‑up testing. This trio forms a solid foundation for recovery.
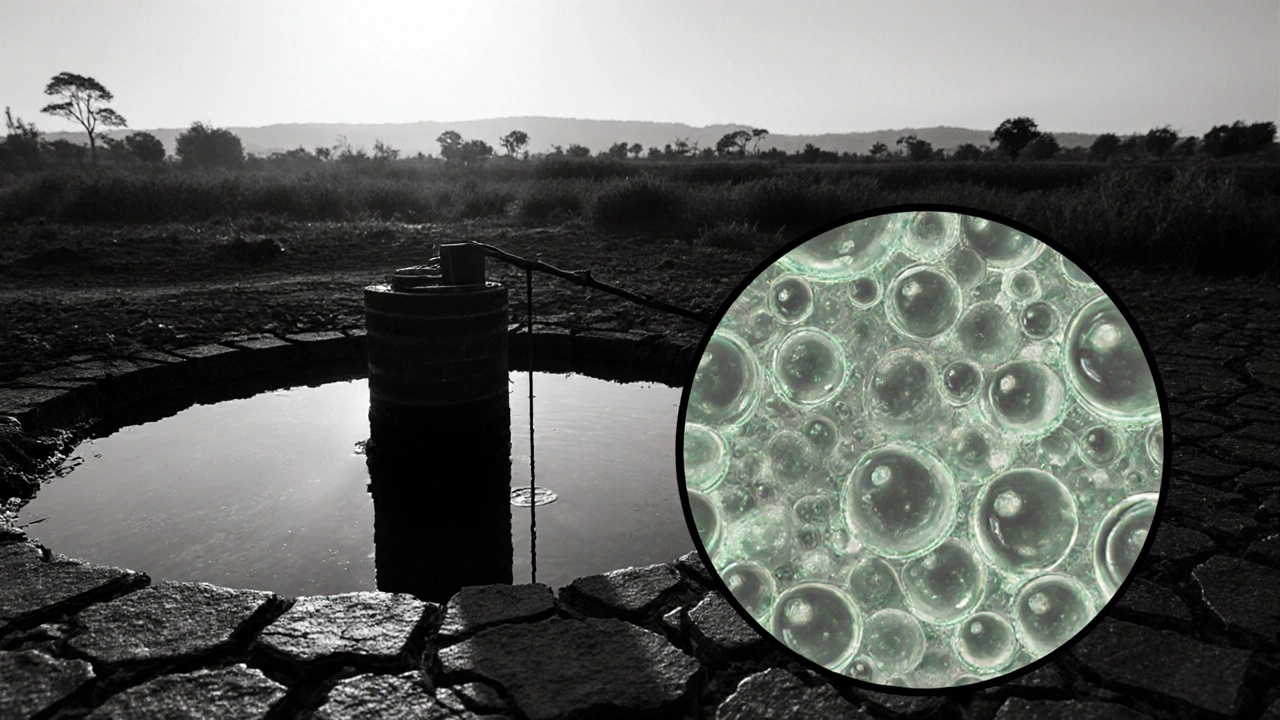
The parasite at the heart of the problem, Entamoeba histolytica, a microscopic protozoan that invades the colon and sometimes the liver, triggers diarrhea, abdominal pain, and fever. Identifying it accurately through stool microscopy or antigen testing is the first step any effective treatment demands. Once confirmed, doctors usually turn to Metronidazole, a nitroimidazole antibiotic that targets invasive amebic tissue as the go‑to drug. Its high cure rate and relatively low cost make it the backbone of most regimens.
Not every case responds to metronidazole alone. For patients with liver abscesses or severe colitis, adding a luminal agent like Paromomycin, an aminoglycoside that stays in the gut to clear residual parasites can prevent recurrence. Some clinicians prefer Tinidazole, a longer‑acting nitroimidazole that allows a shorter course for patients who struggle with adherence. Choosing the right drug influences recovery speed, side‑effect profile, and the chance of a second infection.
Side effects are a real concern, especially for people with liver disease or pregnancy. Metronidazole can cause nausea, metallic taste, and, rarely, neuropathy if taken too long. Tinidazole shares similar issues but often feels easier on the stomach. Paromomycin, being poorly absorbed, mainly causes mild abdominal cramping. Discussing these risks with a healthcare provider helps tailor the regimen to each individual’s health status. Proper dosing—usually 500‑750 mg three times daily for 7‑10 days for metronidazole—ensures the parasite is fully eradicated while keeping adverse events manageable.
After the medication course, confirming eradication is crucial. A repeat stool test two weeks post‑therapy helps catch any lingering infection before it flares again. In cases of hepatic involvement, imaging studies like ultrasound or CT may be repeated to verify abscess resolution. Ongoing hygiene—regular hand‑washing, safe food handling, and clean water—forms the final layer of protection against reinfection.
What You’ll Find Next
The articles below dive deeper into each drug’s dosing nuances, compare side‑effect management strategies, and explore when surgery becomes necessary for complicated liver abscesses. Whether you’re a patient looking for practical tips or a caregiver seeking clear guidance, the collection offers actionable insights to help you navigate amebiasis treatment from diagnosis to full recovery.
Amebiasis Prevention and Treatment: How Governments Protect Public Health
Explore how governments tackle amebiasis through policy, water safety, education, and treatment access, and learn practical steps for effective public‑health action.