Antidepressants for Adolescents – What You Need to Know
When dealing with Antidepressants for Adolescents, medications prescribed to treat depressive disorders in teenagers aged 12‑18. Also known as teen antidepressants, they play a crucial role in managing mood, motivation and school performance. A common class is Selective Serotonin Reuptake Inhibitors (SSRIs), drugs that boost serotonin levels to improve mood, often the first choice for mild to moderate cases. Another important option is Venlafaxine, an SNRI that affects both serotonin and norepinephrine pathways, useful when SSRIs aren’t enough. antidepressants adolescents should never be viewed in isolation; they’re most effective when paired with Psychotherapy, structured counseling that teaches coping skills and emotional regulation. These three entities—medication, therapy, and the teen’s depressive state—form a linked trio that guides any treatment plan.
First, understand Depression in Adolescents, a persistent low mood that interferes with daily activities, school, and relationships. It isn’t just a phase; neurodevelopmental changes make the brain more sensitive to stress, and untreated depression can increase the risk of substance use or self‑harm. Because the teenage brain is still wiring, medication effects can differ from adults—both in effectiveness and side‑effect profile. This reality drives the need for careful dosing: starting low, moving slow, and monitoring weight, sleep, and emotional shifts weekly.
Key Considerations When Prescribing
One semantic triple is clear: Antidepressants for adolescents encompass SSRIs and SNRIs. Another: Effective treatment requires psychotherapy. A third: Side‑effects influence adherence. In practice, clinicians first assess severity using tools like the PHQ‑9‑A, then decide if an SSRI such as fluoxetine or sertraline fits. Fluoxetine remains the only FDA‑approved SSRI for this age group, but clinicians often consider others off‑label based on response and tolerability. When SSRIs fall short, Venlafaxine steps in, though its higher activation risk demands close monitoring for anxiety spikes or agitation.
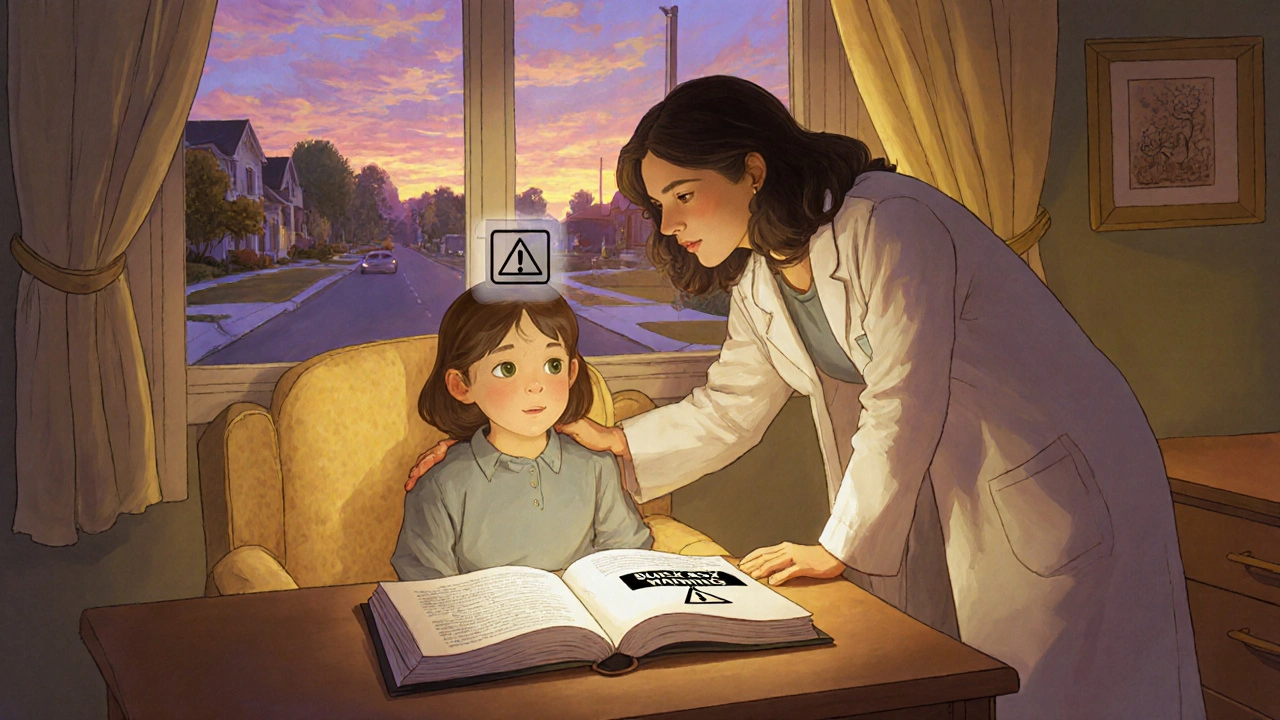
Safety conversations focus on two major concerns: activation (restlessness, insomnia) and suicidal thoughts. Studies show a small increase in suicidal ideation shortly after starting an SSRI, especially in the first few weeks. That’s why a joint plan involving parents, school counselors, and the teen is essential. Regular check‑ins—often weekly for the first month—help catch warning signs early. Additionally, certain side effects like weight gain, sexual dysfunction, or gastrointestinal upset can impact a teen’s willingness to stay on medication, so clinicians must discuss these openly and offer strategies, such as timing doses to minimize daytime sedation.
Beyond medication, integrating psychotherapy amplifies outcomes. Cognitive‑behavioral therapy (CBT) teaches teens how to challenge negative thoughts, while interpersonal therapy (IPT) addresses relationship stressors that often trigger depressive episodes. When both approaches align—medication stabilizing mood chemistry and therapy building coping skills—research shows faster remission and lower relapse rates. The collection of articles below dives deep into each of these points: comparisons of Venlafaxine (Ventodep ER) with other antidepressants, cost and safety analyses of generic Celexa, and broader discussions on teen mental health. Armed with this context, you’ll be ready to explore the detailed guides and make informed choices for adolescent mental health.
Antidepressants for Teens: Black Box Warning, Suicide Risk & Monitoring Guide
Explore the FDA's Black Box Warning on antidepressants for teens, understand the suicide risk, learn monitoring best practices, and see current research on benefits vs. harms.