Driving safety: what to watch when meds or health get involved
Some drugs and health issues don't shout their risks — they sneak up as slower reactions, blurry vision, or sudden dizziness. You probably check your mirrors and tires; add a quick check of your meds and recent symptoms before you drive. Below are clear, useful tips and common troublemakers so you can make safer choices every time you get behind the wheel.
Common meds and conditions that change driving
Seizures are an obvious risk. If you or someone you care for has epilepsy, seizure control and driving rules matter. Our article “Seizures and Sports” explains how to manage activity safely — and many of the same precautions apply to driving: know your seizure-free period required by local law and never drive if you feel a warning aura coming on.
Some antidepressants and sexual health drugs can cause drowsiness or dizziness. For example, bupropion (Wellbutrin) tends to be less sedating than older antidepressants, but side effects vary — read the patient info and ask your prescriber if driving is safe when you start or change dose. Dapoxetine (Priligy) can cause lightheadedness for some people; avoid driving until you know how you react.
Over-the-counter antihistamines, strong pain meds, benzodiazepines, and many sleep aids reduce alertness. Even some heart or blood pressure drugs affect concentration. Diabetes carries its own risk: low blood sugar can cause confusion or blackout. Always test your blood sugar before long drives if you use insulin or meds that can cause hypoglycemia.
Vision matters. Smoking-related eye problems and ocular hypertension can reduce night vision and contrast sensitivity. If you notice glare, narrow vision, or new blurriness, skip driving and get an eye check.
Simple rules to keep you safe on the road
1) Check new meds before you drive. Try them at home first and ask your doctor or pharmacist: “Will this affect my driving?”
2) Watch for warning signs: slowed thinking, fuzzy sight, dizziness, double vision, or sudden sleepiness. If any of these show up, stop driving immediately.
3) Avoid mixing alcohol with meds. Alcohol boosts sedation and reduces reaction time fast.
4) Plan backups. If you start a new treatment or have a bad flare of a chronic condition, arrange a ride, use public transport, or call a friend. Short inconvenience beats a crash.
5) Keep a short log. Note new drugs and any side effects you felt while driving. That helps your prescriber make safer choices next time.
If you want deeper reading, check posts like “Wellbutrin: Benefits, Side Effects, and What to Expect From Bupropion,” “Priligy: Finding the Best Deals,” and “Smoking's Impact on Ocular Hypertension and Eye Health” for more on how specific meds and conditions can affect safety behind the wheel.
Safe driving isn’t just road skills — it’s knowing how your body and medicines behave. A few simple checks before you leave can keep you and others safer, every trip.
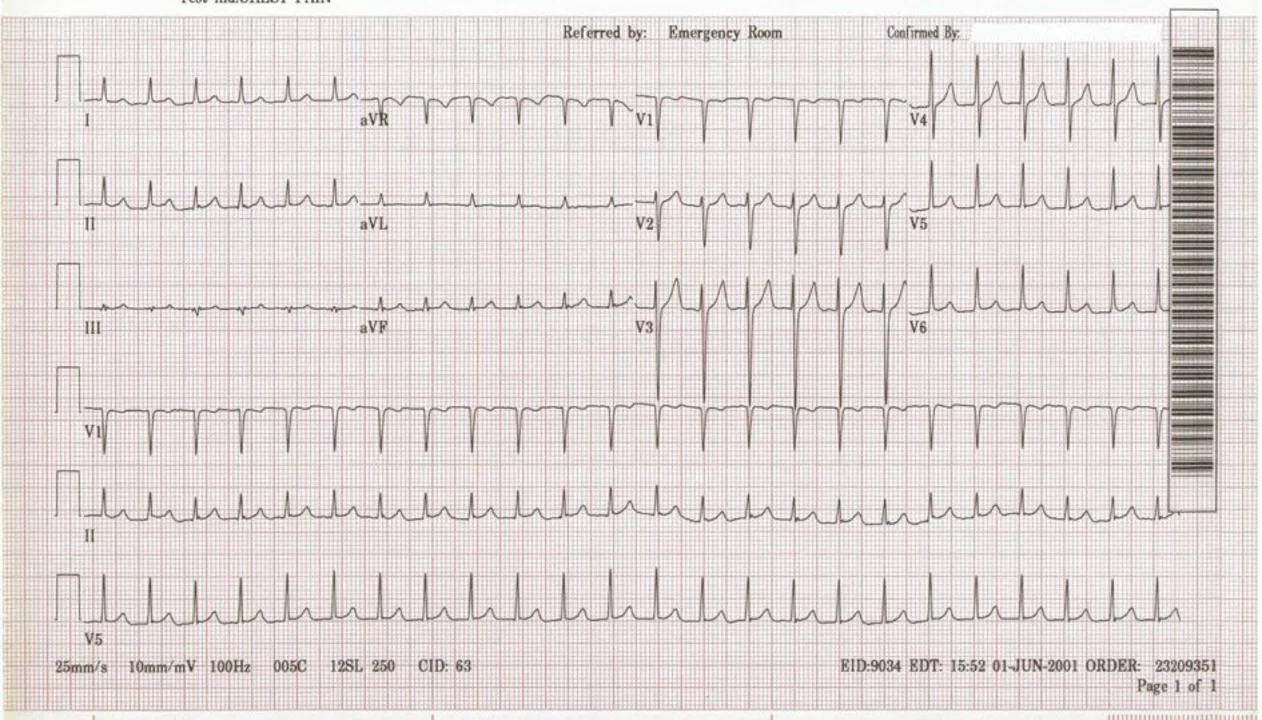
Supraventricular Tachycardia and Driving: Safety Tips and Guidelines
As a blogger, I recently explored the topic of Supraventricular Tachycardia (SVT) and its impact on driving. SVT is a rapid heart rate condition that can cause dizziness, shortness of breath, and even fainting, which can be hazardous while on the road. To ensure a safe driving experience, it's crucial to consult with a healthcare professional and discuss any potential limitations or restrictions related to driving. Additionally, it's essential to take prescribed medications regularly, stay well-hydrated, and avoid triggers such as stress or excessive caffeine intake. By following these guidelines and staying in tune with our bodies, we can continue to enjoy the freedom of the open road while managing SVT effectively.