Embolism Diagnosis: What You Need to Know
When working with embolism diagnosis, the process of spotting clots that block blood flow. Also called clot detection, it’s a critical step in preventing serious complications. The most common forms you’ll hear about are deep vein thrombosis, a clot forming in the leg veins and pulmonary embolism, a clot that travels to the lungs. Doctors usually start with a D-dimer test, a blood test that flags clot‑breakdown fragments and may follow up with imaging like CT pulmonary angiography, a CT scan that visualizes the pulmonary arteries. Understanding how these pieces fit together helps you move quickly from suspicion to treatment.
Key Steps in Evaluating an Embolism
First, clinicians look for warning signs: sudden shortness of breath, chest pain that worsens with a deep breath, rapid heart rate, or swelling in a leg. These symptoms alone don’t confirm an embolism, but they raise the alarm. Next, a quick risk‑factor check is done – recent surgery, long‑haul travel, cancer, or a history of clotting disorders can tip the scales toward a higher suspicion.
Once the suspicion is solid, the embolism diagnosis moves into the lab. A normal D‑dimer often lets doctors rule out a clot without more expensive tests. If the D‑dimer is elevated, imaging steps in. For suspected DVT, a bedside ultrasound of the leg veins is fast and reliable. For a potential pulmonary embolism, CT pulmonary angiography provides a clear picture of any blockage in the lung arteries.
Other imaging tools also play a role. A ventilation‑perfusion (V/Q) scan can be useful when a CT scan isn’t possible due to kidney issues or contrast allergies. Magnetic resonance angiography (MRA) offers a radiation‑free alternative for certain patients, though it’s less common in acute settings.
Lab work isn’t limited to D‑dimer. Blood counts, kidney function tests, and coagulation panels help gauge the patient’s overall health and determine which anticoagulant drugs are safe to use. Knowing a patient’s baseline labs also aids in monitoring treatment response later.
Treatment starts the moment an embolism is confirmed. Anticoagulants like heparin, warfarin, or newer direct oral anticoagulants (DOACs) thin the blood to stop the clot from growing. In severe cases, clot‑busting drugs (thrombolytics) or surgical removal may be necessary. The choice depends on the clot’s size, location, and the patient’s risk profile.
Follow‑up care is just as important as the initial steps. Repeat imaging after a few weeks checks whether the clot is dissolving. Long‑term anticoagulation may be needed for patients with persistent risk factors, while others might only require a short course.
All of these pieces—symptoms, risk factors, lab tests, imaging, and treatment—form a logical chain that drives an accurate embolism diagnosis. Each step builds on the previous one, creating a clear pathway from doubt to decisive action.
Below you’ll find a curated list of articles that dig deeper into each of these topics, from spotting early signs to choosing the right anticoagulant. Keep reading to get practical tips you can apply right away.
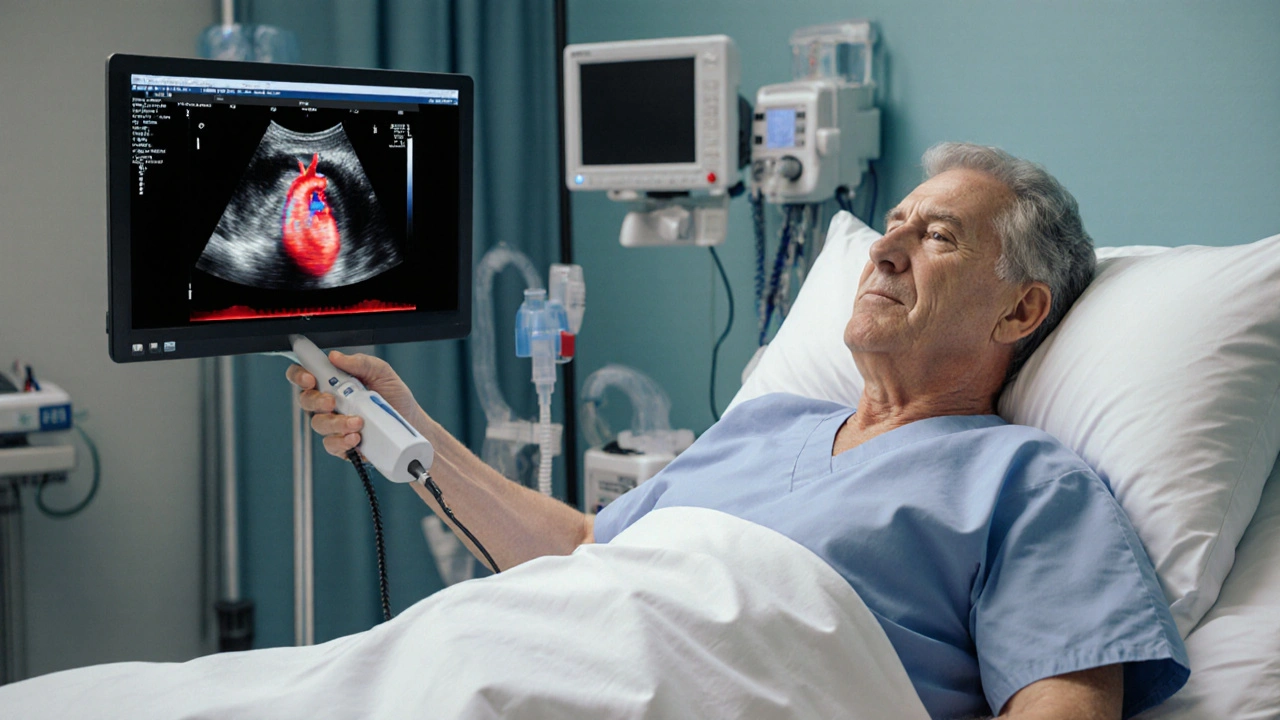
How Echocardiography Guides Embolism Diagnosis and Management
Explore how bedside echocardiography detects clot sources, assesses right‑heart strain, and guides treatment decisions for embolism, with practical tips, comparisons, and FAQs.