P-glycoprotein: How This Protein Affects Your Medications and Why It Matters
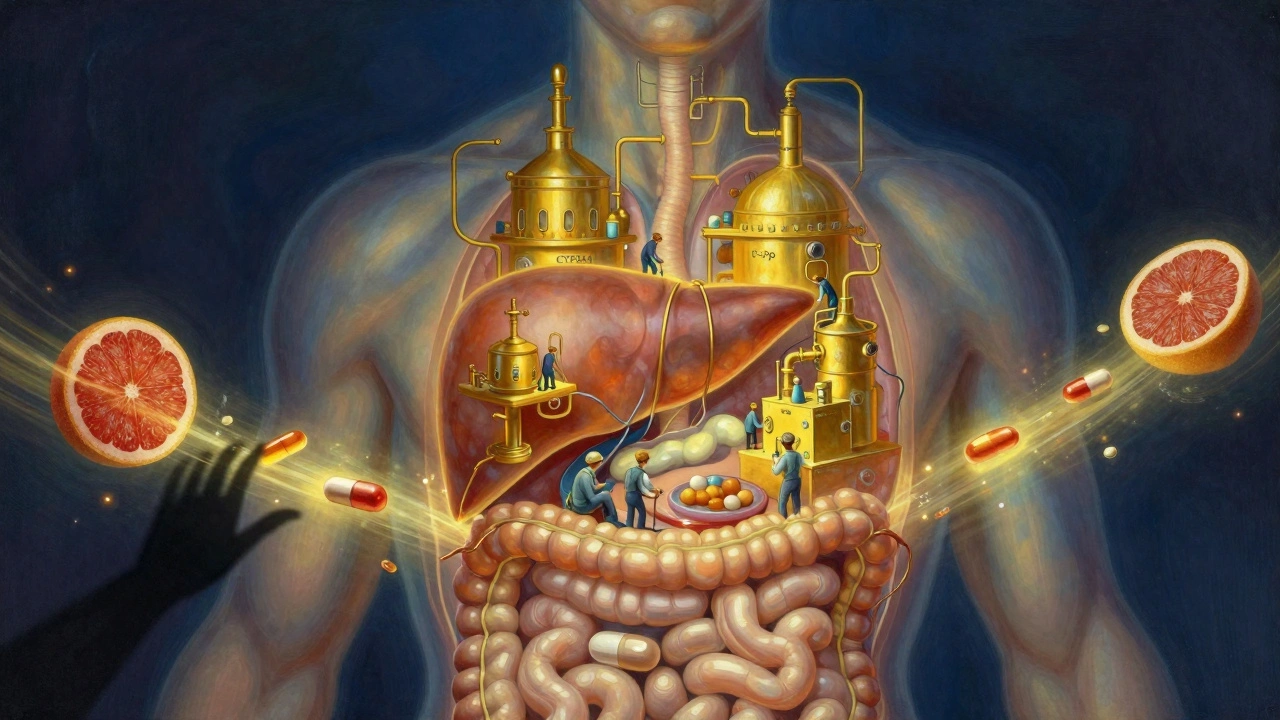
When you take a pill, it doesn’t just go straight to where it’s needed. P-glycoprotein, a transporter protein found in the intestines, liver, kidneys, and blood-brain barrier that pumps certain drugs out of cells. Also known as MDR1, it acts like a bouncer at the door of your cells—letting in what’s safe and kicking out what it thinks is foreign or harmful. This protein is why some medications work for one person but not another, even if they’re on the same dose. If P-glycoprotein is too active, it can flush out drugs like chemotherapy agents, blood thinners, or epilepsy meds before they have a chance to work. If it’s too slow, those same drugs can build up and cause dangerous side effects.
P-glycoprotein doesn’t work alone. It’s tied to pharmacogenomics, the study of how your genes affect how your body responds to drugs. Some people inherit gene variants that make P-glycoprotein overactive, while others have versions that barely function. This explains why two people taking the same drug might have completely different outcomes. It also connects to drug interactions, when one medication blocks or boosts P-glycoprotein’s activity, changing how another drug behaves in the body. Grapefruit juice, for example, can block P-glycoprotein and cause blood levels of certain drugs to spike. On the flip side, St. John’s wort can turn it up, making your meds less effective. Even some antibiotics and antifungals mess with this system.
This isn’t just theory—it shows up in real life. People on blood thinners like warfarin, cancer drugs like paclitaxel, or even heart meds like digoxin have seen their treatment fail because of P-glycoprotein activity. That’s why tracking your meds and talking to your pharmacist about what you’re taking matters. It’s also why some generic drugs don’t work the same way as the brand version—even if they have the same active ingredient. The fillers, coatings, or how the drug is released can change how much gets absorbed, and P-glycoprotein decides what sticks.
What you’ll find in the posts below isn’t just a list of articles. It’s a practical guide to understanding why your meds behave the way they do. From how genetic testing can reveal your P-glycoprotein profile, to how drug shortages and generic substitutions can shift your body’s response, these posts connect the dots between what’s happening inside you and what’s on your prescription bottle. You’ll learn how to spot when your meds aren’t working because of this protein—not because you’re doing something wrong, but because your biology is speaking louder than your doctor’s prescription.
Antiviral Medications and CYP3A4/P-gp Interactions: What You Need to Know
Antiviral medications like those for HIV and hepatitis C can dangerously interact with common drugs through CYP3A4 and P-glycoprotein. Learn how to avoid life-threatening side effects with simple checks and safer treatment options.