TEE vs TTE: A Practical Guide to Cardiac Ultrasound Choices
When evaluating TEE vs TTE, the comparison of transesophageal and transthoracic echocardiography techniques, it helps to first understand the broader field of echocardiography, ultrasound imaging that visualizes the heart's structure and function. This imaging falls under the umbrella of cardiac ultrasound, a non‑invasive tool used to diagnose heart disease. Both TEE and TTE are part of the same diagnostic family, but they differ in how they acquire images, the level of detail they provide, and the situations where each shines.
The first semantic link is simple: TEE vs TTE compares two echocardiography methods. The second link states that echocardiography requires ultrasound waves to create real‑time pictures of the heart. A third connection notes that cardiac ultrasound influences heart disease diagnosis by revealing valve problems, chamber size, and blood flow patterns. Finally, the choice between TEE and TTE often depends on the clinical question—whether you need a quick bedside screen or a detailed view of the posterior structures.
Why the comparison matters for patients and clinicians
Transesophageal echocardiography (TEE), an exam where a probe is gently inserted down the esophagus to get close to the heart delivers high‑resolution images of the left atrium, aortic arch, and valve leaflets. Because the probe sits right behind the heart, TEE can spot small clots, minor leaks, or subtle wall motion abnormalities that a surface scan might miss. However, TEE is semi‑invasive, requires sedation, and isn’t ideal for every patient—especially those with swallowing difficulties or esophageal disease.
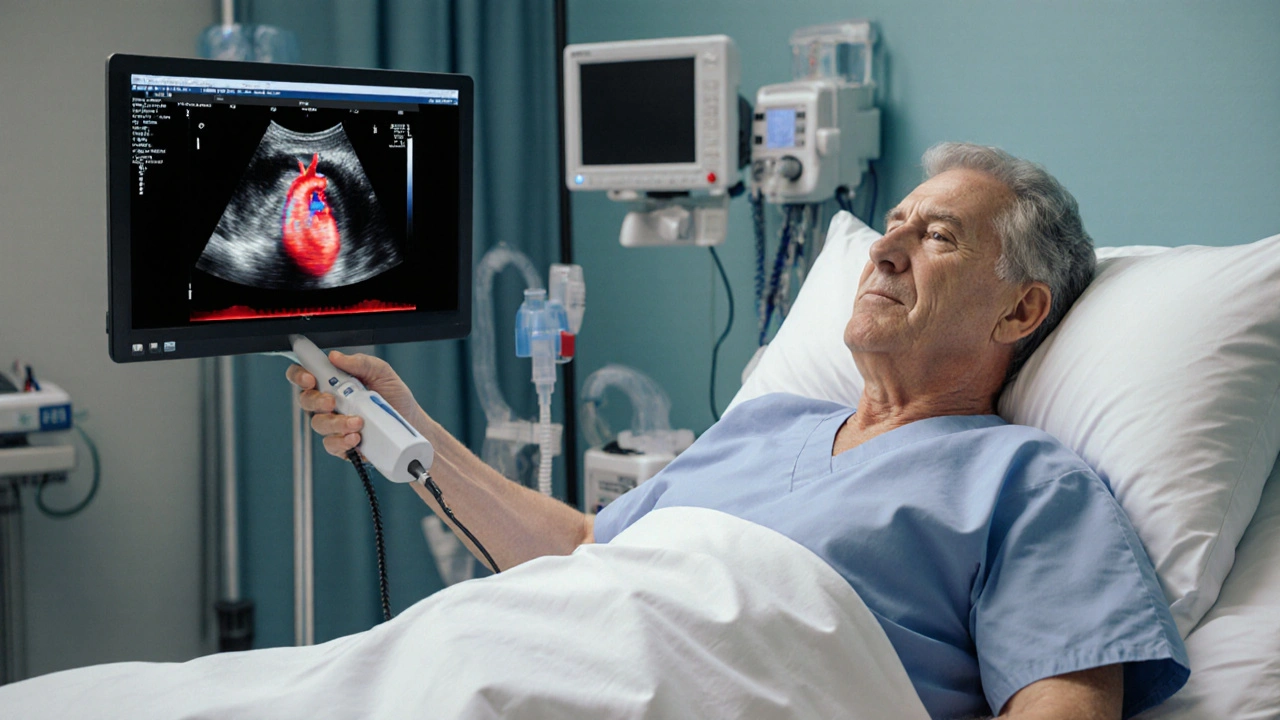
On the other side, Transthoracic echocardiography (TTE), the standard bedside ultrasound performed with a transducer on the chest wall is quick, painless, and can be done in most clinical settings. TTE is the go‑to tool for initial assessment of heart failure, valve function, and congenital anomalies. While its image quality can be limited by obesity, lung tissue, or rib shadows, advances like 3D rendering and contrast agents have narrowed the gap with TEE for many routine exams.
Both techniques share core attributes: they use high‑frequency sound waves, create real‑time movies, and are safe without ionizing radiation. The choice hinges on three main attributes—**invasiveness**, **image clarity**, and **clinical urgency**. For example, a patient with a suspected left atrial thrombus before cardioversion will usually get a TEE because the risk of missing a clot outweighs the discomfort of the probe. Conversely, a patient presenting with shortness of breath and suspected heart failure gets a TTE first to gauge ejection fraction and pressure estimates.
Insurance coverage and procedural cost also play a role. TTE is generally covered as a basic test, while TEE may need prior authorization due to its semi‑invasive nature. This financial aspect can influence decision‑making in outpatient clinics.
When doctors plan a cardiac surgery, they often order both. The TTE provides a broad overview, and the TEE offers a detailed roadmap for the surgeon, especially when operating on the mitral valve or repairing an aortic aneurysm. In the intensive care unit, bedside TTE helps track fluid status, while a later TEE can confirm the source of a newly discovered murmur.
From a patient perspective, knowing the differences can reduce anxiety. Understanding that a TEE involves a short sedation period and that the sensation is brief helps set realistic expectations. Meanwhile, patients appreciate that a TTE can be performed while they sit up and talk to the technician.
Technology continues to blur the lines. Portable handheld TTE devices now fit in a pocket, allowing clinicians to perform quick scans in the field or emergency department. At the same time, 4‑D TEE offers dynamic imaging that can guide percutaneous procedures like left atrial appendage closure.
In summary, TEE vs TTE isn’t a competition but a complementary partnership. Each method brings unique strengths that, when combined, give a full picture of heart health. Whether you’re a patient prepping for an exam or a clinician choosing the right tool, the key is to match the test to the clinical question, patient tolerance, and resource availability.
Below you’ll find a curated set of articles that dive deeper into specific scenarios—how to prepare for a TEE, interpreting TTE results for heart failure, comparing costs, and more. These resources will help you decide which imaging approach fits your needs and answer the practical questions that often come up when dealing with cardiac ultrasound.
How Echocardiography Guides Embolism Diagnosis and Management
Explore how bedside echocardiography detects clot sources, assesses right‑heart strain, and guides treatment decisions for embolism, with practical tips, comparisons, and FAQs.